When COVID-19 affects muscle: effects of quarantine in older adults
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 16 May 2020
Authors
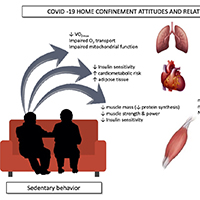
At the beginning of 2020 a respiratory diseased named COVID-19 rapidly spread worldwide. Due to the presence of comorbidities and a greater susceptibility to infections, older adults are the population most affected by this pandemic. An efficient pharmacological treatment for COVID-19 is not ready yet; in the meanwhile, a general quarantine has been initiated as a preventive action against the spread of the disease. If on one side this countermeasure is slowing the spread of the virus, on the other side is also reducing the amount of physical activity. Sedentariness is associated with numerous negative health outcomes and increase risk of fall, fractures and disabilities in older adults. Models of physical inactivity have been widely studied in the past decades, and most studies agreed that is necessary to implement physical exercise (such as walking, low load resistance or in bed exercise) during periods of disuse to protect muscle mass and function from catabolic crisis. Moreover, older adults have a blunted response to physical rehabilitation, and a combination of intense resistance training and nutrition are necessary to overcome the loss of in skeletal muscle due to disuse.






