Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
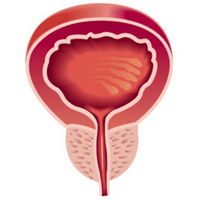
Visceral adiposity is associated with worse urinary and sexual function recovery after radical prostatectomy: Results from a longitudinal cohort study
Objective: A prospective longitudinal cohort study on the impact of anthropometric measures on the sexual function and continence recovery in patients treated with laparoscopic radical prostatectomy (LRP) is presented.
Material and methods: Anthropometric measures, International Index of Erectile Function (IIEF-5) and International Prostatic Symptoms Score questionnaires, were collected before surgery and at the end of follow-up period. All patients were assigned into the following groups: A) non-obese; B) non-obese with central adiposity; C) obese without central adiposity; D) obese with central adiposity. Urinary and sexual functions were the outcome measures.
Results: At the end of follow-up, in 29 patients with visceral adiposity (VA) the median IIEF-5 was 14 (IQR 7-18) while in 49 non-VA patients (62.8%) was 22 (IQR 17-24) (p < 0.001). Twenty-three patients (79.3%) with VA reported complete continence, while 6 (20.7%) used ≥ 2 pads per day. Forty-eight patients (97.9%) without VA reported complete continence. VA was confirmed as a strong independent predictor for worse continence (HR 3.67; 2.75-4.51 CI95% p = 0.003) and sexual function recovery (HR: 4.51; 3.09-5.63 CI95% p < 0.001).
Conclusion: We truly believe obese with visceral adiposity patients with prostate cancer should receive detailed preoperative counseling before surgery, including higher risk of suboptimal functional outcomes.
Downloads
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/aiua.2021.3.285
https://doi.org/10.4081/aiua.2021.3.285