Concomitant high-risk pulmonary embolism and subdural hematoma: endo-vascular system thrombolysis as a possible solution to a difficult challenge
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 22 September 2023
Authors
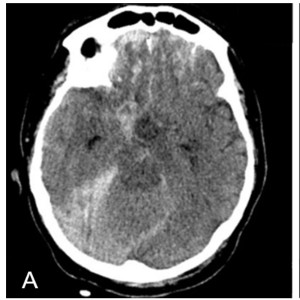
Acute pulmonary embolism (PE) is a challenging and potentially fatal cardiovascular disorder. In high-risk patients, percutaneous catheter embolectomy may be considered when thrombolysis is contraindicated or has failed. We hereby discuss the case of a 60-year-old man who was found unconscious on the ground with signs of head trauma and respiratory failure. He was found to have a massive pulmonary embolism and multiple basilar skull fractures associated with slight subdural and subarachnoid hemorrhages. His acute treatment required a multidisciplinary discussion and approach. EkoSonic™ Endovascular System (EKOS) thrombolysis was successfully performed. The patient required intensive care unit (ICU) monitoring and treatment for 31 days. Upon discharge, henoxaparin 4000 UI twice per day was prescribed as anticoagulant, without any evidence of pulmonary hypertension or severe neurological sequelae.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.











