Immunoexpression of p53 mutant-type in Iranian patients with primary and recurrence oral squamous cell carcinoma
Accepted: 10 October 2022
HTML: 9
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
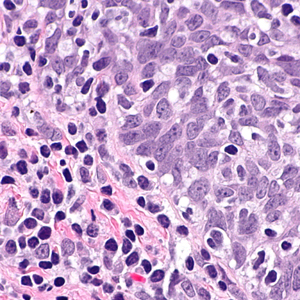
Mutations in tumor suppressor p53 protein can occur at different phases of malignant transformation and affect the patient's prognosis. This study aimed to evaluate the expression of mutant p53 protein in Iranian patients with the primary and recurrence oral squamous cell carcinoma (OSCC). This retrospective cross-sectional study conducted on a group of patients with the primary OSCC (n=122) and the control subjects with oral noncancerous reactive lesions (n=80). Immunohistochemistry was performed with the DO-7 monoclonal antibody against p53 protein, and samples with ≥10% immunostaining were considered positive. Statistical analyses were carried out using SPSS. Positive staining for p53 was observed in none of the control subjects and 57.4% (70 of 122) of the primary OSCC patients (p<0.0001, OR=107.69, 95%CI=6.49-179.0). The p53 immunopositivity had no significant differences between males and females (54.2% vs. 62%, p=0.390), but significantly different between those aged below and over 50 years (p<0.0001, OR=4.52, 95%CI=1.07-12.05). During follow-up, OSCC recurrence occurred in 104 patients, but the phenotype of the mutant p53 protein in patients who relapsed was the same as in matched primary tumors (p=0.763). Risk of recurrence had no significant differences between p53-positive and p53-negative cases (p=0.953), males and females (p=0.263), and age below and over 50 years (p=0.223). Despite its confirmed diagnostic value, the immunoexpression of the p53 mutant protein in OSCC in cancer recurrence was the same as in the primary tumor. However, further studies with a larger sample size and longer follow-up are needed to confirm or change our conclusions.
Wang SW, Chan LP, Wang LF, Wu CW, Lin SH, Huang TY, Lee KW. Secondary primary malignancy in patients with head and neck squamous cell carcinoma: 27-year experience from the perspective of diagnostic tools. PLoS One. 2022 Feb 15;17(2):e0263773. DOI: https://doi.org/10.1371/journal.pone.0263773
Chow LQM. Head and Neck Cancer. N Engl J Med. 2020 Jan 2;382(1):60-72. DOI: https://doi.org/10.1056/NEJMra1715715
Sun Z, Sun X, Chen Z, Du J, Wu Y. Head and Neck Squamous Cell Carcinoma: Risk Factors, Molecular Alterations, Immunology and Peptide Vaccines. Int J Pept Res Ther. 2022;28(1):19. Epub 2021 Dec 8. DOI: https://doi.org/10.1007/s10989-021-10334-5
Singh MP, Kumar V, Agarwal A, Kumar R, Bhatt ML, Misra S. Clinico-epidemiological study of oral squamous cell carcinoma: A tertiary care centre study in North India. J Oral Biol Craniofac Res. 2016 Jan-Apr;6(1):31-4. Epub 2015 Dec 4. DOI: https://doi.org/10.1016/j.jobcr.2015.11.002
Taghavi N, Yazdi I. Prognostic factors of survival rate in oral squamous cell carcinoma: clinical, histologic, genetic and molecular concepts. Arch Iran Med. 2015 May;18(5):314-9.
Markopoulos AK. Current aspects on oral squamous cell carcinoma. Open Dent J. 2012;6:126-30. Epub 2012 Aug 10. DOI: https://doi.org/10.2174/1874210601206010126
Wang B, Zhang S, Yue K, Wang XD. The recurrence and survival of oral squamous cell carcinoma: a report of 275 cases. Chin J Cancer. 2013 Nov;32(11):614-8. Epub 2013 Apr 19. DOI: https://doi.org/10.5732/cjc.012.10219
Beck TN, Golemis EA. Genomic insights into head and neck cancer. Cancers Head Neck. 2016;1:1. doi: 10.1186/s41199-016-0003-z. Epub 2016 Jun 3. DOI: https://doi.org/10.1186/s41199-016-0003-z
Pai SI, Westra WH. Molecular pathology of head and neck cancer: implications for diagnosis, prognosis, and treatment. Annu Rev Pathol. 2009;4:49-70. DOI: https://doi.org/10.1146/annurev.pathol.4.110807.092158
Perdomo S, Anantharaman D, Foll M, Abedi-Ardekani B, Durand G, Reis Rosa LA, Holmila R, Le Calvez-Kelm F, Tajara EH, Wünsch-Filho V, Levi JE, Vilensky M, Polesel J, Holcatova I, Simonato L, Canova C, Lagiou P, McKay JD, Brennan P. Genomic analysis of head and neck cancer cases from two high incidence regions. PLoS One. 2018 Jan 29;13(1):e0191701. DOI: https://doi.org/10.1371/journal.pone.0191701
Zhou G, Liu Z, Myers JN. TP53 Mutations in Head and Neck Squamous Cell Carcinoma and Their Impact on Disease Progression and Treatment Response. J Cell Biochem. 2016 Dec;117(12):2682-2692. Epub 2016 Jun 3. DOI: https://doi.org/10.1002/jcb.25592
Feroz W, Sheikh AMA. Exploring the multiple roles of guardian of the genome: P53. Egyptian J Med Human Gen. 2020;21(1):49. DOI: https://doi.org/10.1186/s43042-020-00089-x
Mijit M, Caracciolo V, Melillo A, Amicarelli F, Giordano A. Role of p53 in the Regulation of Cellular Senescence. Biomolecules. 2020 Mar 8;10(3):420. DOI: https://doi.org/10.3390/biom10030420
Chen J. The Cell-Cycle Arrest and Apoptotic Functions of p53 in Tumor Initiation and Progression. Cold Spring Harb Perspect Med. 2016 Mar 1;6(3):a026104. DOI: https://doi.org/10.1101/cshperspect.a026104
Castellanos MR, Pan Q. Novel p53 therapies for head and neck cancer. World J Otorhinolaryngol Head Neck Surg. 2016 Jul 19;2(2):68-75. DOI: https://doi.org/10.1016/j.wjorl.2016.05.005
de Bakker T, Journe F, Descamps G, Saussez S, Dragan T, Ghanem G, Krayem M, Van Gestel D. Restoring p53 Function in Head and Neck Squamous Cell Carcinoma to Improve Treatments. Front Oncol. 2022 Jan 6;11:799993. PMID: 35071005; PMCID: PMC8770810. DOI: https://doi.org/10.3389/fonc.2021.799993
Chin D, Boyle GM, Theile DR, Parsons PG, Coman WB. Molecular introduction to head and neck cancer (HNSCC) carcinogenesis. Br J Plast Surg. 2004 Oct;57(7):595-602. PMID: 15380692. DOI: https://doi.org/10.1016/j.bjps.2004.06.010
Fakhrjou A, Seyed Outounchi Sj. Morphologic Evaluation of P53 Apoptotic Signaling Responses and Proliferative Activity of Ki-67 in Oral Lichen Planus, Oral Squamous Cell Carcinoma and Normal Specimens. J Med Sci. 2012;12(2):51-6. DOI: https://doi.org/10.3923/jms.2012.51.56
Farhadi S, Shahsavari F, Alf K. Comparison of Expression of p53 and bcl-2 Markers in Oral Lichen Planus and Oral Squamous Cell Carcinoma. J Res Dent Maxillofac Sci 2018; 3 (2) :37-45. DOI: https://doi.org/10.29252/jrdms.3.2.37
Etemad-Moghadam S, Keyhani A, Yazdani K, Alaeddini M. Status of p53 and p27(KIP1) in Iranian Patients With Oral Squamous Cell Carcinoma. Iran Red Crescent Med J. 2015 Oct 19;17(10):e19359. DOI: https://doi.org/10.5812/ircmj.19359
Agha-Hosseini F, Mirzaii-Dizgah I, Miri-Zarandi N. Unstimulated salivary p53 in patients with oral lichen planus and squamous cell carcinoma. Acta Med Iran. 2015 Jul;53(7):439-43.
Sina M, Pedram M, Ghojazadeh M, Kochaki A, Aghbali A. P53 gene codon 72 polymorphism in patients with oral squamous cell carcinoma in the population of northern Iran. Med Oral Patol Oral Cir Bucal. 2014 Nov 1;19(6):e550-5. DOI: https://doi.org/10.4317/medoral.19794
Pinholt EM, Rindum J, Pindborg JJ. Oral cancer: a retrospective study of 100 Danish cases. Br J Oral Maxillofac Surg. 1997 Apr;35(2):77-80. DOI: https://doi.org/10.1016/S0266-4356(97)90679-3
Anneroth G, Batsakis J, Luna M. Review of the literature and a recommended system of malignancy grading in oral squamous cell carcinomas. Scand J Dent Res. 1987 Jun;95(3):229-49. DOI: https://doi.org/10.1111/j.1600-0722.1987.tb01836.x
Casalini P, Iorio MV, Berno V, Bergamaschi A, Børresen Dale AL, Gasparini P, Orlandi R, Casati B, Tagliabue E, Ménard S. Relationship between p53 and p27 expression following HER2 signaling. Breast. 2007 Dec;16(6):597-605. Epub 2007 Jun 28. DOI: https://doi.org/10.1016/j.breast.2007.05.007
Sarr P, A D, Faye O, M S, B M, Kane Y, et al. Association of the TP53 Arg72Pro Polymorphism with Oral Squamous Cell Carcinoma: A Meta-Analysis. J Mol Genet Med. 2020;14(3):455. DOI: https://doi.org/10.37421/jmgm.2020.14.455
Liu R, Sun K, Wang Y, Jiang Y, Kang J, Ma H. The effects of proliferating cell nuclear antigen and p53 in patients with oral squamous cell carcinoma: a systematic review and meta-analysis. Ann Transl Med. 2021 Dec;9(23):1739. DOI: https://doi.org/10.21037/atm-21-6133
Ozaki T, Nakagawara A. Role of p53 in Cell Death and Human Cancers. Cancers (Basel). 2011 Mar 3;3(1):994-1013. DOI: https://doi.org/10.3390/cancers3010994
Marei HE, Althani A, Afifi N, Hasan A, Caceci T, Pozzoli G, Morrione A, Giordano A, Cenciarelli C. p53 signaling in cancer progression and therapy. Cancer Cell Int. 2021 Dec 24;21(1):703. DOI: https://doi.org/10.1186/s12935-021-02396-8
Kato K, Kawashiri S, Yoshizawa K, Kitahara H, Okamune A, Sugiura S, Noguchi N, Yamamoto E. Expression form of p53 and PCNA at the invasive front in oral squamous cell carcinoma: correlation with clinicopathological features and prognosis. J Oral Pathol Med. 2011 Oct;40(9):693-8. Epub 2011 Apr 18. DOI: https://doi.org/10.1111/j.1600-0714.2011.01032.x
Carlos de Vicente J, Junquera Gutiérrez LM, Zapatero AH, Fresno Forcelledo MF, Hernández-Vallejo G, López Arranz JS. Prognostic significance of p53 expression in oral squamous cell carcinoma without neck node metastases. Head Neck. 2004 Jan;26(1):22-30. DOI: https://doi.org/10.1002/hed.10339
Monteiro LS, Diniz-Freitas M, Garcia-Caballero T, Warnakulasuriya S, Forteza J, Fraga M. Combined cytoplasmic and membranous EGFR and p53 overexpression is a poor prognostic marker in early stage oral squamous cell carcinoma. J Oral Pathol Med. 2012 Aug;41(7):559-67. Epub 2012 Mar 14. DOI: https://doi.org/10.1111/j.1600-0714.2012.01142.x
Abrahao AC, Bonelli BV, Nunes FD, Dias EP, Cabral MG. Immunohistochemical expression of p53, p16 and hTERT in oral squamous cell carcinoma and potentially malignant disorders. Braz Oral Res. 2011 Jan-Feb;25(1):34-41. PMID: 21359449. DOI: https://doi.org/10.1590/S1806-83242011000100007
Fan CC, Wang TY, Cheng YA, Jiang SS, Cheng CW, Lee AY, Kao TY. Expression of E-cadherin, Twist, and p53 and their prognostic value in patients with oral squamous cell carcinoma. J Cancer Res Clin Oncol. 2013 Oct;139(10):1735-44. Epub 2013 Aug 30. DOI: https://doi.org/10.1007/s00432-013-1499-9
Mneimneh WS, Xu B, Ghossein C, Alzumaili B, Sethi S, Ganly I, Khimraj A, Dogan S, Katabi N. Clinicopathologic Characteristics of Young Patients with Oral Squamous Cell Carcinoma. Head Neck Pathol. 2021 Dec;15(4):1099-1108. Epub 2021 Apr 2. DOI: https://doi.org/10.1007/s12105-021-01320-w
Santos HB, dos Santos TK, Paz AR, Cavalcanti YW, Nonaka CF, Godoy GP, Alves PM. Clinical findings and risk factors to oral squamous cell carcinoma in young patients: A 12-year retrospective analysis. Med Oral Patol Oral Cir Bucal. 2016 Mar 1;21(2):e151-6. DOI: https://doi.org/10.4317/medoral.20770
Mineta H, Borg A, Dictor M, Wahlberg P, Akervall J, Wennerberg J. p53 mutation, but not p53 overexpression, correlates with survival in head and neck squamous cell carcinoma. Br J Cancer. 1998 Oct;78(8):1084-90. DOI: https://doi.org/10.1038/bjc.1998.632
Nylander K, Stenling R, Gustafsson H, Zackrisson B, Roos G. p53 expression and cell proliferation in squamous cell carcinomas of the head and neck. Cancer. 1995 Jan 1;75(1):87-93. DOI: https://doi.org/10.1002/1097-0142(19950101)75:1<87::AID-CNCR2820750115>3.0.CO;2-V
Perisanidis C, Perisanidis B, Wrba F, Brandstetter A, El Gazzar S, Papadogeorgakis N, Seemann R, Ewers R, Kyzas PA, Filipits M. Evaluation of immunohistochemical expression of p53, p21, p27, cyclin D1, and Ki67 in oral and oropharyngeal squamous cell carcinoma. J Oral Pathol Med. 2012 Jan;41(1):40-6. Epub 2011 Aug 29. DOI: https://doi.org/10.1111/j.1600-0714.2011.01071.x
Frank JL, Bur ME, Garb JL, Kay S, Ware JL, Sismanis A, Neifeld JP. p53 tumor suppressor oncogene expression in squamous cell carcinoma of the hypopharynx. Cancer. 1994 Jan 1;73(1):181-6. DOI: https://doi.org/10.1002/1097-0142(19940101)73:1<181::AID-CNCR2820730131>3.0.CO;2-3
Jalali MM, Heidarzadeh A, Zavarei MJ, Sarmast H. p53 overexpression impacts on the prognosis of laryngeal squamous cell carcinomas. Asian Pac J Cancer Prev. 2011;12(7):1731-4.
Geisler SA, Olshan AF, Weissler MC, Cai J, Funkhouser WK, Smith J, Vick K. p16 and p53 Protein expression as prognostic indicators of survival and disease recurrence from head and neck cancer. Clin Cancer Res. 2002 Nov;8(11):3445-53.
Zhang C, Liu J, Xu D, Zhang T, Hu W, Feng Z. Gain-of-function mutant p53 in cancer progression and therapy. J Mol Cell Biol. 2020 Sep 1;12(9):674-687. doi: 10.1093/jmcb/mjaa040. DOI: https://doi.org/10.1093/jmcb/mjaa040
Roszkowska KA, Gizinski S, Sady M, Gajewski Z, Olszewski MB. Gain-of-Function Mutations in p53 in Cancer Invasiveness and Metastasis. Int J Mol Sci. 2020 Feb 17;21(4):1334. DOI: https://doi.org/10.3390/ijms21041334
Chen Y, Xu L, Massey L, Zlotolow I, Huvos A, Garinchesa P, Old L. Frameshift and nonsense p53 mutations in squamous-cell carcinoma of head and neck - non-reactivity with 3 anti-p53 monoclonal-antibodies. Int J Oncol. 1994 Mar;4(3):609-14. DOI: https://doi.org/10.3892/ijo.4.3.609
Copyright (c) 2022 The Authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.


 https://doi.org/10.4081/ejtm.2022.10847
https://doi.org/10.4081/ejtm.2022.10847



