Delayed splenic rupture after a minor blunt trauma: A case report and literature review
Accepted: 1 September 2022
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
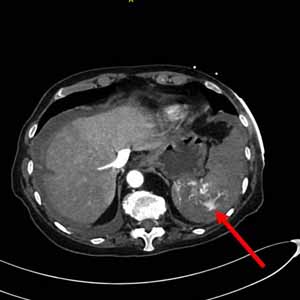
Delayed Splenic Rupture (DSR) is a rare but well-known manifestation of Blunt Splenic Injury (BSI), which most commonly occurs following a car accident, a fall from a great height, or a direct blow to the left thorax or abdomen. If the history of trauma is remote or unknown, the diagnosis can be difficult or missed, and a high index of suspicion is not warranted. Regardless of the time and mechanism of the inciting event, DSR should be considered in the differential diagnosis of an acute surgical abdomen. We present a case of DSR in an 81-year-old woman caused by a remote minor blunt abdominal trauma four weeks prior to her admission to our emergency department for acute abdominal pain and hemorrhagic shock (ATLS CLASS III). Starting with this case report, we conducted a literature review on the subject in order to raise awareness, knowledge, and understanding of DSR among emergency clinicians.
Sosada K, Wiewiora M, Piecuch J. Literature review of non-operative management of patients with blunt splenic injury: impact of splenic artery embolization. Videosurg Other Miniinvasive Tech 2014;9:309e14. DOI: https://doi.org/10.5114/wiitm.2014.44251
Olsen WR, Polley TZ. A second look at delayed splenic rupture. Arch Surg 1977;112:422–5 DOI: https://doi.org/10.1001/archsurg.1977.01370040074012
Baudet R. Ruptures de la rate. Medicine Practique 1907;3:565–7
McIndoe AH. Delayed hemorrhage following traumatic rupture of the spleen. Br J Surg 1932;20:249–68. DOI: https://doi.org/10.1002/bjs.1800207809
Kluger Y, Paul DB, Raves JJ, et al. Delayed rupture of the spleen–myths, facts, and their importance case reports and literature review. J Trauma 1994;36:568–71. DOI: https://doi.org/10.1097/00005373-199404000-00019
Furlan A, Tublin ME, Rees MA, et al. Delayed splenic vascular injury after non-operative management of blunt splenic trauma. J Surg Res 2017;211:87–94. DOI: https://doi.org/10.1016/j.jss.2016.11.062
Freiwald S: Late-presenting complications after splenic trauma. Perm J 2010;14:41-4. DOI: https://doi.org/10.7812/TPP/09-101
Farhat GA, Abdu RA, Vanek VW. Delayed splenic rupture: real or imaginary? Am Surg 1992;58:340–5.
Aubrey-Bassler FK, Sowers N. 613 cases of splenic rupture without risk factors or previously diagnosed disease: a systematic review. BMC Emerg Med 2012;12:11 DOI: https://doi.org/10.1186/1471-227X-12-11
Simpson RA, Ajuwon R. Occult splenic injury: delayed presentation manifesting as jaundice. Emerg Med J 2001;18:504 –5. DOI: https://doi.org/10.1136/emj.18.6.504
Hiraide A, Yamamoto H, Yahata K, et al. Delayed rupture of the spleen caused by an intrasplenic pseudoaneurysm following blunt trauma: case report. J Trauma 1994;36:743–4 DOI: https://doi.org/10.1097/00005373-199405000-00026
Tintinalli JE, Kelen GD, Stapczynski JS: Emergency Medicine: A Comprehensive Study Guide. McGraw Hill, New York; 2004.
Pittet D, Randel-Frausto S, Li N, et al. Systemic inflammatory response syndrome, sepsis, severe sepsis and septic shock: incidence, morbidities and outcomes in surgical ICU patients. Intensive Care Med 1995;21:302–9. DOI: https://doi.org/10.1007/BF01705408
Rotstein OD. Modeling the two-hit hypothesis for evaluating strategies to prevent organ injury after shock/resuscitation. J Trauma 2003;54:S203–6. DOI: https://doi.org/10.1097/01.TA.0000064512.62949.92
Adams JM, Hauser CJ, Livingston DH, Lavery RF, Fekete Z, Deitch EA. Early trauma polymorphonuclear neutrophil responses to chemokines are associated with development of sepsis, pneumonia, and organ failure. J Trauma 2001;51:452–6. DOI: https://doi.org/10.1097/00005373-200109000-00005
Roumen RM, Hendriks T, Ven-Jongekrijg J, et al. Cytokine patterns in patients after major vascular surgery, hemorrhagic shock, and severe blunt trauma. Relation with subsequent adult respiratory distress syndrome and multiple organ failure. Ann Surg 1993;218:769–76. DOI: https://doi.org/10.1097/00000658-199312000-00011
American College of Surgeon’s Commitee on Trauma. Advanced Trauma Life Support® (ATLS®) Student manual 9th ed.ed., American College of Surgeon, Chicago; 2012.
Carr JA, Roiter C, Alzuhaili A. Correlation of operative and pathological injury grade with computed tomographic grade in the failed nonoperative management of blunt splenic trauma. Eur J Trauma Emerg Surg 2012;38:433–8. DOI: https://doi.org/10.1007/s00068-012-0179-9
Kirkpatrick AW, Sirois M, Laupland KB, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the extended focused assessment with sonography for trauma (EFAST). J Trauma 2004;57:288–95. DOI: https://doi.org/10.1097/01.TA.0000133565.88871.E4
Doody O, Lyburn D, Geoghegan T, et al. Blunt trauma to the spleen: ultrasonographic findings. Clin Radiol 2005;60:968–76. DOI: https://doi.org/10.1016/j.crad.2005.05.005
El-Matbouly M, Jabbour G, El-Menyar A, et al. Blunt splenic trauma: assessment, management and outcomes. Surgeon. 2016;14:52–8. DOI: https://doi.org/10.1016/j.surge.2015.08.001
Morell-Hofert D, Primavesi F, Fodor M, et al. Validation of the revised 2018 AAST-OIS classification and the CT severity index for prediction of operative management and survival in patients with blunt spleen and liver injuries. Eur Radiol 2020;30:6570–81 DOI: https://doi.org/10.1007/s00330-020-07061-8
Coccolini F, Montori G, Catena F, et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg 2017;12:40. DOI: https://doi.org/10.1186/s13017-017-0151-4
Roy P, Mukherjee R, Parik M. Splenic trauma in the twenty-first century: Changing trends in management. Ann Royal Coll Surg Engl 2018;100:650–6. DOI: https://doi.org/10.1308/rcsann.2018.0139
Olthof DC, Joosse P, van der Vlies CH, et al. Prognostic factors for failure of nonoperative management in adults with blunt splenic injury: a systematic review. J Trauma Acute Care Surg 2013;74:546–557. DOI: https://doi.org/10.1097/TA.0b013e31827d5e3a
Cocanour CS. Blunt splenic injury. Curr Opin Crit Care 2010;16:575–81. DOI: https://doi.org/10.1097/MCC.0b013e3283402f3a
Zarzaur BL, Vashi S, Magnotti LJ, et al. The real risk of splenectomy after discharge home following nonoperative management of blunt splenic injury. J Trauma 2009;66:1531–8. DOI: https://doi.org/10.1097/TA.0b013e3181a4ed11
Renzulli P, Hostettler A, Schoepfer AM, et al. Systematic review of atraumatic splenic rupture. Br J Surg 2009;96:1114–21. DOI: https://doi.org/10.1002/bjs.6737
Weinberg JA, Magnotti LJ, Croce MA, et al. The utility of serial computed tomography imaging of blunt splenic injury: still worth a second look? J Trauma 2007;62:1143–1148 DOI: https://doi.org/10.1097/TA.0b013e318047b7c2
Stassen NA, Bhullar I, Cheng JD, et al. Selective non-operative management of blunt splenic injury. J Trauma Acute Care Surg 2012;73:294–300. DOI: https://doi.org/10.1097/TA.0b013e3182702afc
Olthof DC, Van der Vlies CH, Joosse P, et al. Consensus strategies for the nonoperative management of patients with blunt splenic injury. J Trauma Acute Care Surg 2013;74:1567–74. DOI: https://doi.org/10.1097/TA.0b013e3182921627
Liu S, Lei J, Zeng Z, Zhang Y. Management of traumatic splenic rupture in adults: a single center’s experience in mainland China. Hepatogastroenterology 2014;61:966–71.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ecj.2022.10822
https://doi.org/10.4081/ecj.2022.10822