Dental implants in Sjögren syndrome
Accepted: 16 February 2020
HTML: 79
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
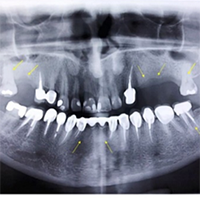
Sjögren's syndrome (SS) is a complex autoimmune disease that predominantly affects the exocrine glands, notably the salivary and lacrimal glands, resulting in dryness of the mucosa recognized as xerostomia. Chief oral complications reported by patients consist of high caries rate, burning sensation of the mucosa, early tooth loss, intensified tooth wear and repetitive failure of dental restorations. In particular, due to the decreased salivary flow, conventional removable prostheses might irritate the mucosa and lead to painful ulcerations at the borders of the denture. Implant-supported prostheses offer a unique solution to the difficulties experienced by edentulous patients with Sjögren’s syndrome. This research showed no signs of peri-implantitis or peri-implant mucositis during 7-years following the placement of implants. The present study indicates that successful long-term maintenance of dental implants can be also achieved in SS patients.
Reale M, D'Angelo C, Costantini E, et al. MicroRNA in Sjogren's Syndrome: Their Potential Roles in Pathogenesis and Diagnosis. J Immunol Res 2018; 2018:7510174. 10.1155/2018/7510174. DOI: https://doi.org/10.1155/2018/7510174
Ji J, Sundquist J, Sundquist K. Gender-specific incidence of autoimmune diseases from national registers. J Autoimmun 2016; 69:102-6. 10.1016/j.jaut.2016.03.003. DOI: https://doi.org/10.1016/j.jaut.2016.03.003
Almeida D, Vianna K, Arriaga P, et al. Dental implants in Sjogren's syndrome patients: A systematic review. PLoS One 2017; 12:e0189507. 10.1371/journal.pone.0189507. DOI: https://doi.org/10.1371/journal.pone.0189507
Vivino FB. Sjogren's syndrome: Clinical aspects. Clin Immunol 2017; 182:48-54. 10.1016/j.clim.2017.04.005. DOI: https://doi.org/10.1016/j.clim.2017.04.005
Brito-Zeron P, Ramos-Casals M, group E-Stf. Advances in the understanding and treatment of systemic complications in Sjogren's syndrome. Curr Opin Rheumatol 2014; 26:520-7. 10.1097/BOR.0000000000000096. DOI: https://doi.org/10.1097/BOR.0000000000000096
Mathews SA, Kurien BT, Scofield RH. Oral manifestations of Sjogren's syndrome. J Dent Res 2008; 87:308-18. 10.1177/154405910808700411. DOI: https://doi.org/10.1177/154405910808700411
Seifi Kafshgari H, Yazdanian, M., Ranjbar, R., Tahmasebi, E., Mirsaeed, S., Tebyanian, H., Ebrahimzadeh, M. A., & Goli, H. R. . The effect of Citrullus colocynthis extracts on Streptococcus mutans, Candida albicans, normal gingival fibroblast and breast cancer cells. J Biol Res 2019; 92. 10.4081/jbr.2019.8201. DOI: https://doi.org/10.4081/jbr.2019.8201
Goules AV, Tzioufas AG. Primary Sjogren's syndrome: clinical phenotypes, outcome and the development of biomarkers. Immunol Res 2017; 65:331-44. 10.1007/s12026-016-8844-4. DOI: https://doi.org/10.1007/s12026-016-8844-4
Cornec D, Jamin C, Pers JO. Sjogren's syndrome: where do we stand, and where shall we go? J Autoimmun 2014; 51:109-14. 10.1016/j.jaut.2014.02.006. DOI: https://doi.org/10.1016/j.jaut.2014.02.006
Albrecht K, Callhoff J, Westhoff G, et al. The Prevalence of Dental Implants and Related Factors in Patients with Sjogren Syndrome: Results from a Cohort Study. J Rheumatol 2016; 43:1380-5. 10.3899/jrheum.151167. DOI: https://doi.org/10.3899/jrheum.151167
Dawes C, Pedersen AM, Villa A, et al. The functions of human saliva: A review sponsored by the World Workshop on Oral Medicine VI. Arch Oral Biol 2015; 60:863-74. 10.1016/j.archoralbio.2015.03.004. DOI: https://doi.org/10.1016/j.archoralbio.2015.03.004
Karami A, Tebyanian H, Barkhordari A, et al. Healing effects of ointment drug on full-thickness wound. C R Acad Bulg Sci 2019; 72:123-9. DOI: https://doi.org/10.7546/CRABS.2019.01.16
Pedersen AM, Bardow A, Nauntofte B. Salivary changes and dental caries as potential oral markers of autoimmune salivary gland dysfunction in primary Sjogren's syndrome. BMC Clin Pathol 2005; 5:4. 10.1186/1472-6890-5-4. DOI: https://doi.org/10.1186/1472-6890-5-4
Jorkjend L, Johansson A, Johansson A, et al. Periodontitis, caries and salivary factors in Sjögren's syndrome patients compared to sex‐ and age‐matched controls. Journal of Oral Rehabilitation 2003; 30:369-78. 10.1046/j.1365-2842.2003.01088.x DOI: https://doi.org/10.1046/j.1365-2842.2003.01088.x
Chochlidakis K, Ercoli C, Elad S. Challenges in implant-supported dental treatment in patients with Sjogren's syndrome: A case report and literature review. Quintessence Int 2016; 47:515-24. 10.3290/j.qi.a36009.
Krennmair G, Seemann R, Piehslinger E. Dental implants in patients with rheumatoid arthritis: clinical outcome and peri-implant findings. J Clin Periodontol 2010; 37:928-36. 10.1111/j.1600-051X.2010.01606.x. DOI: https://doi.org/10.1111/j.1600-051X.2010.01606.x
Binon PP. Thirteen-year follow-up of a mandibular implant-supported fixed complete denture in a patient with Sjogren's syndrome: a clinical report. J Prosthet Dent 2005; 94:409-13. 10.1016/j.prosdent.2005.09.010. DOI: https://doi.org/10.1016/j.prosdent.2005.09.010
Pjetursson BE, Lang NP. Sinus floor elevation utilizing the transalveolar approach. Periodontol 2000 2014; 66:59-71. 10.1111/prd.12043. DOI: https://doi.org/10.1111/prd.12043
Esposito M, Grusovin MG, Chew YS, et al. One-stage versus two-stage implant placement. A Cochrane systematic review of randomised controlled clinical trials. Eur J Oral Implantol 2009; 2:91-9.
Soufdoost RS, Yazdanian M, Tahmasebi E, et al. In vitro and in vivo evaluation of novel Tadalafil/β-TCP/Collagen scaffold for bone regeneration: A rabbit critical-size calvarial defect study. Biocybernetics and Biomedical Engineering 2019. https://doi.org/10.1016/j.bbe.2019.07.003. DOI: https://doi.org/10.1016/j.bbe.2019.07.003
Esfahanizadeh N, Daneshparvar P, Takzaree N, et al. Histologic Evaluation of the Bone Regeneration Capacities of Bio-Oss and MinerOss X in Rabbit Calvarial Defects. Int J Periodontics Restorative Dent 2019; 39:e219-e27. DOI: https://doi.org/10.11607/prd.4181
Klokkevold PR, Han TJ, Camargo PM. Aesthetic management of extractions for implant site development: delayed versus staged implant placement. Pract Periodontics Aesthet Dent 1999; 11:603-10; quiz 12.
Veitz-Keenan A. Marginal bone loss and dental implant failure may be increased in smokers. Evidence-based dentistry 2016; 17:6-7. 10.1038/sj.ebd.6401145. DOI: https://doi.org/10.1038/sj.ebd.6401145
Negri BM, Pimentel SP, Casati MZ, et al. Impact of a chronic smoking habit on the osteo-immunoinflammatory mediators in the peri-implant fluid of clinically healthy dental implants. Arch Oral Biol 2016; 70:55-61. 10.1016/j.archoralbio.2016.05.014. DOI: https://doi.org/10.1016/j.archoralbio.2016.05.014
Esfahanizadeh N, Yousefi H. Successful Implant Placement in a Case of Florid Cemento-Osseous Dysplasia: A Case Report and Literature Review. J Oral Implantol 2018; 44:275-9. 10.1563/aaid-joi-D-17-00140. DOI: https://doi.org/10.1563/aaid-joi-D-17-00140
Mori G, Kobayashi T, Ito T, et al. Implant-supported Prostheses in Patient with Sjogren's Syndrome: Clinical Report with 3-year Follow-up. The Bulletin of Tokyo Dental College 2018; 59:201-6. 10.2209/tdcpublication.2017-0036. DOI: https://doi.org/10.2209/tdcpublication.2017-0036
Shakeri F, Tebyanian H, Karami A, et al. Effect of Topical Phenytoin on Wound Healing. Trauma Mon 2017; 22:e35488. https://doi.org/10.5812/traumamon.35488. DOI: https://doi.org/10.5812/traumamon.35488
Babavalian H, Latifi AM, Shokrgozar MA, et al. Cloning and expression of recombinant human platelet-derived growth factor-BB in Pichia Pink. Cell Mol Biol (Noisy-le-grand) 2016; 62:45-51. https://doi.org/10.14715/cmb/2016.62.8.8. DOI: https://doi.org/10.14715/cmb/2016.62.8.8
Hessling SA, Wehrhan F, Schmitt CM, et al. Implant-based rehabilitation in oncology patients can be performed with high long-term success. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons 2015; 73:889-96. 10.1016/j.joms.2014.11.009. DOI: https://doi.org/10.1016/j.joms.2014.11.009
Celenligil H, Eratalay K, Kansu E, et al. Periodontal status and serum antibody responses to oral microorganisms in Sjogren's syndrome. Journal of periodontology 1998; 69:571-7. 10.1902/jop.1998.69.5.571. DOI: https://doi.org/10.1902/jop.1998.69.5.571
Khomarlou N, Aberoomand-Azar P, Lashgari AP, et al. Essential oil composition and in vitro antibacterial activity of Chenopodium album subsp. striatum. Acta Biologica Hungarica 2018; 69:144-55. https://doi.org/10.1556/018.69.2018.2.4. DOI: https://doi.org/10.1556/018.69.2018.2.4
Mosaddad SA, Tahmasebi E, Yazdanian A, et al. Oral microbial biofilms: an update. European Journal of Clinical Microbiology & Infectious Diseases 2019. 10.1007/s10096-019-03641-9. DOI: https://doi.org/10.1007/s10096-019-03641-9
Esfahanizadeh N, Nourani Mohammad R, Bahador A, et al. The Anti-biofilm Activity of Nanometric Zinc doped Bioactive Glass against Putative Periodontal Pathogens: An in vitro Study. Biomedical Glasses2018. p. 95. DOI: https://doi.org/10.1515/bglass-2018-0009
Esfahanizadeh N, Mirmalek SP, Bahador A, et al. Formation of biofilm on various implant abutment materials. Gen Dent 2018; 66:39-44.
Jepsen S, Berglundh T, Genco R, et al. Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol 2015; 42 Suppl 16:S152-7. 10.1111/jcpe.12369. DOI: https://doi.org/10.1111/jcpe.12369
Costa FO, Takenaka-Martinez S, Cota LO, et al. Peri-implant disease in subjects with and without preventive maintenance: a 5-year follow-up. J Clin Periodontol 2012; 39:173-81. 10.1111/j.1600-051X.2011.01819.x. DOI: https://doi.org/10.1111/j.1600-051X.2011.01819.x
Pavlakis PP, Alexopoulos H, Kosmidis ML, et al. Peripheral neuropathies in Sjogren's syndrome: a critical update on clinical features and pathogenetic mechanisms. J Autoimmun 2012; 39:27-33. 10.1016/j.jaut.2012.01.003. DOI: https://doi.org/10.1016/j.jaut.2012.01.003
Isidor F, Brøndum K, Hansen H, et al. Outcome of treatment with implant-retained dental prostheses in patients with Sjögren syndrome. Int J Oral Maxillofac Implants 1999; 14:736-43.
Payne AG, Lownie JF, Van Der Linden WJ. Implant-supported prostheses in patients with Sjogren's syndrome: a clinical report on three patients. Int J Oral Maxillofac Implants 1997; 12:679-85.
Oczakir C, Balmer S, Mericske-Stern R. Implant-prosthodontic treatment for special care patients: a case series study. The International journal of prosthodontics 2005; 18:383-9.
Spinato S, Soardi CM, Zane AM. A mandibular implant-supported fixed complete dental prosthesis in a patient with Sjogren syndrome: case report. Implant Dent 2010; 19:178-83. 10.1097/ID.0b013e3181dbe081. DOI: https://doi.org/10.1097/ID.0b013e3181dbe081
Weinlander M, Krennmair G, Piehslinger E. Implant prosthodontic rehabilitation of patients with rheumatic disorders: a case series report. The International journal of prosthodontics 2010; 23:22-8.
Ergun S, Katz J, Cifter ED, et al. Implant-supported oral rehabilitation of a patient with systemic lupus erythematosus: case report and review of the literature. Quintessence Int 2010; 41:863-7.
Peron C, Javed F, Romanos GE. Immediate Loading of Tantalum-Based Implants in Fresh Extraction Sockets in Patient With Sjogren Syndrome: A Case Report and Literature Review. Implant Dent 2017; 26:634-8. 10.1097/id.0000000000000594. DOI: https://doi.org/10.1097/ID.0000000000000594
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejtm.2020.8811
https://doi.org/10.4081/ejtm.2020.8811



