Pain in child patients: A review on managements
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 15 December 2019
Authors
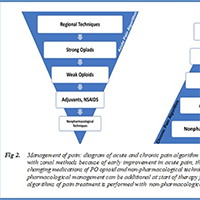
Pain has been known as one of the major universal health concerns about ill children, because of its morbidity and potential mortality. Pain suitable evaluation is a challenge in children because the verbalization is difficult. Low clinical information, few pediatric researches, and the worry of opioid side effects make difficult to provide satisfactory treatments. Many pharmacologic and non-pharmacologic strategies to manage pain exist for pediatric pain treatment. The purpose of this review article is to describe exhaustively pain mechanism, evaluation and management by review literature from January 2000 to January 2019 using PubMed, EMBASE, MEDLINE, LILACS databases. Pharmacological and integrative non-pharmacological therapies has been indicated in acute and chronic pain treatment. Opioids and opioid-sparing agents target nociceptive and neuropathic pain. With due attention to available results, an early combination of pharmacological and integrative non pharmacological treatments are indicated in children pain management.






