Effects of N-acetylcysteine and metformin treatment on the stereopathological characteristics of uterus and ovary
Accepted: 16 February 2022
HTML: 10
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
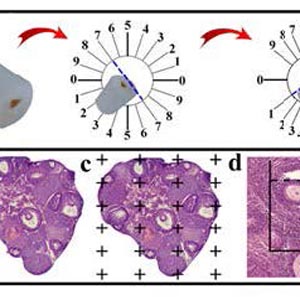
In this study, the stereo-pathological effect of metformin and N-acetyl cysteine is evaluated on the uterus and ovary of polycystic ovary syndrome (PCOS) mice. 96 mature females (8-weekold, weight of 20–30 gr) BALB/c mice were classified into 6 groups including the control group (n= 16), letrozole-induced PCOS group (n=16), PCOS + metformin (n=16), PCOS+NAC (n=16) and a separate control group for NAC (n=16). Another PCOS group was maintained for a month to make sure that features remain till the end of the study. Testosterone level, vaginal cytology and stereological evaluations were assessed. Vaginal cytology in letrozole-receiving mice showed a diestrus phase continuity. Testosterone level, body weight, uterine weight, endometrial volume, myometrial volume, gland volume, stromal volume, epithelial volume, vessel volume, daughter and conglomerate glands, endometrial thickness, and myometrial thickness exhibited an increasing trend in the uterus of PCOS mice. While normal gland and vessel length decreased in the PCOS group. Ovarian volume, corticomedullary volume, primary follicles, secondary follicles, and ovarian cysts were increased in PCOS ovaries. While corpus luteum, primordial, graafian, and atretic follicles showed a decline in the PCOS group. NAC and metformin, however, managed to restore the condition to normal. Given the prevalence of PCOS and its impact on fertility, the use of noninvasive methods is of crucial significance. NAC can control and treat pathological parameters and help as a harmless drug in the treatment of women with PCOS.
Escobar-Morreale HF. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nature Reviews Endocrinology. 2018;14(5):270-84. Epub 2018 Mar 23. DOI: https://doi.org/10.1038/nrendo.2018.24
Azziz R, Carmina E, Chen Z, Dunaif A, Laven JS, Legro RS, et al. Polycystic ovary syndrome. Nature reviews Disease primers. 2016;2(1):1-18. DOI: https://doi.org/10.1038/nrdp.2016.57
Amato G, Conte M, Mazziotti G, Lalli E, Vitolo G, Tucker AT, et al. Serum and follicular fluid cytokines in polycystic ovary syndrome during stimulated cycles. Obstetrics & Gynecology. 2003;101(6):1177-82. DOI: https://doi.org/10.1097/00006250-200306000-00009
Indhavivadhana S, Rattanachaiyanont M, Wongwananuruk T, Techatraisak K, Tanmahasamut P, Dangrat C. Brief communication (Original). Hyperandrogenemia is associated with thin endometrium in reproductive-aged Thai women with polycystic ovary syndrome. Asian Biomedicine. 2013;7(4):545-51.
Kitaya K, Matsubayashi H, Yamaguchi K, Nishiyama R, Takaya Y, Ishikawa T, et al. Chronic endometritis: potential cause of infertility and obstetric and neonatal complications. American Journal of Reproductive Immunology. 2016;75(1):13-22. Epub 2015 Oct 18. DOI: https://doi.org/10.1111/aji.12438
Komal F, Khan MK, Imran M, Ahmad MH, Anwar H, Ashfaq UA, et al. Impact of different omega-3 fatty acid sources on lipid, hormonal, blood glucose, weight gain and histopathological damages profile in PCOS rat model. Journal of Translational Medicine. 2020;18(1):1-11. DOI: https://doi.org/10.1186/s12967-020-02519-1
Huang Y, Yu Y, Gao J, Li R, Zhang C, Zhao H, et al. Impaired oocyte quality induced by dehydroepiandrosterone is partially rescued by metformin treatment. PloS one. 2015;10(3):e0122370. DOI: https://doi.org/10.1371/journal.pone.0122370
Di Pietro M, Parborell F, Irusta G, Pascuali N, Bas D, Bianchi MS, et al. Metformin regulates ovarian angiogenesis and follicular development in a female polycystic ovary syndrome rat model. Endocrinology. 2015;156(4):1453-63. Epub 2015 Jan 15. DOI: https://doi.org/10.1210/en.2014-1765
Ahmadi Shokooh S, Azadbakht M. The effect of L-carnitine and metformin on histomorphology characteristics of uterus in mice with polycystic ovary. Biharean Biologist. 2020;14(1):16-24.
Zhai J, Yao G-D, Wang J-Y, Yang Q-L, Wu L, Chang Z-Y, et al. Metformin regulates key microRNAs to improve endometrial receptivity through increasing implantation marker gene expression in patients with PCOS undergoing IVF/ICSI. Reproductive Sciences. 2019;26(11):1439-48. Epub 2019 Jan 1. DOI: https://doi.org/10.1177/1933719118820466
Sandhu JK, Waqar A, Jain A, Joseph C, Srivastava K, Ochuba O, Alkayyali T, Ruo SW, Poudel S. Oxidative Stress in Polycystic Ovarian Syndrome and the Effect of Antioxidant N-Acetylcysteine on Ovulation and Pregnancy Rate. Cureus. 2021 Sep 11;13(9):e17887. DOI: https://doi.org/10.7759/cureus.17887
Kamalipour F, Jalali H, Azarnia M. Comparison the Effect of Metformin and Clomiphene Citrate on Sirtuin3 gene Expression in the Oocytes of Mice with Polycystic Ovary Syndrome. Iranian Journal of Pharmaceutical Research: IJPR. 2020;19(4):160.
Gonzalez G. Determining the stage of the estrous cycle in female mice by vaginal smear. Cold Spring Harbor Protocols. 2016;2016(8):pdb. prot094474. DOI: https://doi.org/10.1101/pdb.prot094474
Mühlfeld C, Nyengaard JR, Mayhew TM. A review of state-of-the-art stereology for better quantitative 3D morphology in cardiac research. Cardiovascular Pathology. 2010;19(2):65-82. Epub 2009 Jan 14. DOI: https://doi.org/10.1016/j.carpath.2008.10.015
Sá SI, Maia J, Bhowmick N, Silva SM, Silva A, Correia-da-Silva G, et al. Uterine histopathological changes induced by acute administration of tamoxifen and its modulation by sex steroid hormones. Toxicology and Applied Pharmacology. 2019;363:88-97. Epub 2018 Nov 29. DOI: https://doi.org/10.1016/j.taap.2018.11.015
Dorph‐Petersen KA, Nyengaard J, Gundersen H. Tissue shrinkage and unbiased stereological estimation of particle number and size. Journal of microscopy. 2001;204(3):232-46. DOI: https://doi.org/10.1046/j.1365-2818.2001.00958.x
Pappalardo M, Vita R, Di Bari F, Le Donne M, Trimarchi F, Benvenga S. Gly972Arg of IRS-1 and Lys121Gln of PC-1 polymorphisms act in opposite way in polycystic ovary syndrome. Journal of Endocrinological Investigation. 2017;40(4):367-76. Epub 2016 Oct 26. DOI: https://doi.org/10.1007/s40618-016-0569-7
Elia E, Vighi S, Lombardi E, Motta AB. Detrimental effects of hyperandrogenism on uterine functions. International immunopharmacology. 2008;8(13-14):1827-34. Epub 2008 Sep 24. DOI: https://doi.org/10.1016/j.intimp.2008.09.002
Ferrando RE, Nyengaard JR, Hays SR, Fahy JV, Woodruff PG. Applying stereology to measure thickness of the basement membrane zone in bronchial biopsy specimens. Journal of allergy and clinical immunology. 2003;112(6):1243-5. DOI: https://doi.org/10.1016/j.jaci.2003.09.038
Noorafshan A, Ahmadi M, Mesbah S-F, Karbalay-Doust S. Stereological study of the effects of letrozole and estradiol valerate treatment on the ovary of rats. Clinical and Experimental Reproductive Medicine. 2013;40(3):115. Epub 2013 Sep 30. DOI: https://doi.org/10.5653/cerm.2013.40.3.115
Karbalay-Doust S, Noorafshan A. Stereological estimation of ovarian oocyte volume, surface area and number: application on mice treated with nandrolone decanoate. Folia histochemica et cytobiologica. 2012;50(2):275-9. DOI: https://doi.org/10.5603/FHC.2012.0037
Hayes MG, Urbanek M, Ehrmann DA, Armstrong LL, Lee JY, Sisk R, et al. Genome-wide association of polycystic ovary syndrome implicates alterations in gonadotropin secretion in European ancestry populations. Nature communications. 2015;6(1):1-13. Erratum in: Nat Commun. 2016;7:10762. Erratum in: Nat Commun. 2020 Apr 28;11(1):2158.
Cassar S, Misso ML, Hopkins WG, Shaw CS, Teede HJ, Stepto NK. Insulin resistance in polycystic ovary syndrome: a systematic review and meta-analysis of euglycaemic–hyperinsulinaemic clamp studies. Human reproduction. 2016;31(11):2619-31. Epub 2016 Oct 7. DOI: https://doi.org/10.1093/humrep/dew243
Walters K, Bertoldo M, Handelsman D. Evidence from animal models on the pathogenesis of PCOS. Best Practice & Research Clinical Endocrinology & Metabolism. 2018;32(3):271-81. Epub 2018 Mar 31. DOI: https://doi.org/10.1016/j.beem.2018.03.008
Kauffman AS, Thackray VG, Ryan GE, Tolson KP, Glidewell-Kenney CA, Semaan SJ, et al. A novel letrozole model recapitulates both the reproductive and metabolic phenotypes of polycystic ovary syndrome in female mice. Biology of reproduction. 2015;93(3):69, 1-12. Epub 2015 Jul 22. DOI: https://doi.org/10.1095/biolreprod.115.131631
Ryan GE, Malik S, Mellon PL. Antiandrogen treatment ameliorates reproductive and metabolic phenotypes in the letrozole-induced mouse model of PCOS. Endocrinology. 2018;159(4):1734-47. DOI: https://doi.org/10.1210/en.2017-03218
Carmina E, Rosato F, Janni A. Extensive clinical experience. relative prevalence of different androgen excess disorders in 950 women referred because of clinical hyperandrogenism. 2006;91:2-6. Epub 2005 Nov 1. DOI: https://doi.org/10.1210/jc.2005-1457
Xu J, Dun J, Yang J, Zhang J, Lin Q, Huang M, et al. Letrozole rat model mimics human polycystic ovarian syndrome and changes in insulin signal pathways. Medical science monitor: international medical journal of experimental and clinical research. 2020;26:e923073-1. DOI: https://doi.org/10.12659/MSM.923073
Dumesic DA, Oberfield SE, Stener-Victorin E, Marshall JC, Laven JS, Legro RS. Scientific statement on the diagnostic criteria, epidemiology, pathophysiology, and molecular genetics of polycystic ovary syndrome. Endocrine reviews. 2015;36(5):487-525. DOI: https://doi.org/10.1210/er.2015-1018
Abbott DH, Bacha F. Ontogeny of polycystic ovary syndrome and insulin resistance in utero and early childhood. Fertility and sterility. 2013;100(1):2-11. DOI: https://doi.org/10.1016/j.fertnstert.2013.05.023
Kelley ST, Skarra DV, Rivera AJ, Thackray VG. The gut microbiome is altered in a letrozole-induced mouse model of polycystic ovary syndrome. PloS one. 2016;11(1):e0146509. DOI: https://doi.org/10.1371/journal.pone.0146509
Manneras L, Cajander S, Holmäng A, Seleskovic Z, Lystig T, Lönn M, et al. A new rat model exhibiting both ovarian and metabolic characteristics of polycystic ovary syndrome. Endocrinology. 2007;148(8):3781-91. Epub 2007 May 10. DOI: https://doi.org/10.1210/en.2007-0168
Rezvanfar MA, Shojaei Saadi HA, Gooshe M, Abdolghaffari AH, Baeeri M, Abdollahi M. Ovarian aging-like phenotype in the hyperandrogenism-induced murine model of polycystic ovary. Oxidative medicine and cellular longevity. 2014;2014. Epub 2014 Feb 19. DOI: https://doi.org/10.1155/2014/948951
Brawer JR, Munoz M, Farookhi R. Development of the polycystic ovarian condition (PCO) in the estradiol valerate-treated rat. Biology of reproduction. 1986;35(3):647-55. DOI: https://doi.org/10.1095/biolreprod35.3.647
Leeman L, Acharya U. The use of metformin in the management of polycystic ovary syndrome and associated anovulatory infertility: the current evidence. Journal of Obstetrics and Gynaecology. 2009;29(6):467-72. DOI: https://doi.org/10.1080/01443610902829414
Poretsky L, Clemons J, Bogovich K. Hyperinsulinemia and human chorionic gonadotropin synergistically promote the growth of ovarian follicular cysts in rats. Metabolism. 1992;41(8):903-10. DOI: https://doi.org/10.1016/0026-0495(92)90175-A
Kireev R, Tresguerres A, Garcia C, Borras C, Ariznavarreta C, Vara E, et al. Hormonal regulation of pro-inflammatory and lipid peroxidation processes in liver of old ovariectomized female rats. Biogerontology. 2010;11(2):229-43. Epub 2009 Jul 26. DOI: https://doi.org/10.1007/s10522-009-9242-2
Nabiuni M, Ghafurniyan H, Azarnia M, Karimzadeh L. The Effect of Green Tea Extract on Reproductive Improvement in Estradiol Valerate-Induced Polycystic Ovary Polycystic Ovarian Syndrome in Rat. Iranian Journal of Pharmaceutical Research. 2015;14(4):1215-23.
Stracquadanio M, Ciotta L, Palumbo M. Relationship between serum anti-Mullerian hormone and intrafollicular AMH levels in PCOS women. Gynecological Endocrinology. 2018;34(3):223-8. Epub 2017 Sep 23. DOI: https://doi.org/10.1080/09513590.2017.1381838
Matsuda F, Inoue N, Manabe N, Ohkura S. Follicular growth and atresia in mammalian ovaries: regulation by survival and death of granulosa cells. Journal of Reproduction and Development. 2012;58(1):44-50. DOI: https://doi.org/10.1262/jrd.2011-012
Dumesic DA, Richards JS. Ontogeny of the ovary in polycystic ovary syndrome. Fertility and sterility. 2013;100(1):23-38. DOI: https://doi.org/10.1016/j.fertnstert.2013.02.011
Agarwal SK, Judd HL, Magoffin DA. A mechanism for the suppression of estrogen production in polycystic ovary syndrome. The Journal of Clinical Endocrinology & Metabolism. 1996;81(10):3686-91. DOI: https://doi.org/10.1210/jcem.81.10.8855823
Smith P, Steckler TL, Veiga-Lopez A, Padmanabhan V. Developmental programming: differential effects of prenatal testosterone and dihydrotestosterone on follicular recruitment, depletion of follicular reserve, and ovarian morphology in sheep. Biology of reproduction. 2009;80(4):726-36. DOI: https://doi.org/10.1095/biolreprod.108.072801
Hillier SG, Ross GT. Effects of exogenous testosterone on ovarian weight, follicular morphology and intraovarian progesterone concentration in estrogen-primed hypophysectomized immature female rats. Biology of Reproduction. 1979;20(2):261-8. DOI: https://doi.org/10.1095/biolreprod20.2.261
Franks S, Stark J, Hardy K. Follicle dynamics and anovulation in polycystic ovary syndrome. Human reproduction update. 2008;14(4):367-78. doi: 10.1093/humupd/dmn015. Epub 2008 May 22. Erratum in: Hum Reprod Update. 2008 Sep-Oct;14(5):539. DOI: https://doi.org/10.1093/humupd/dmn015
Bandariyan E, Mogheiseh A, Ahmadi A. Study of Body Weight and Histomorphometry of Uterus in Experimentally Polycystic Ovary Syndrome Induced by Dehydroepiandrosterone in Mouse Models Treated with Lutein. Journal of Veterinary Research. 2021;76(2):242-9.
Giudice LC. Endometrium in PCOS: implantation and predisposition to endocrine CA. Best practice & research Clinical endocrinology & metabolism. 2006;20(2):235-44. DOI: https://doi.org/10.1016/j.beem.2006.03.005
Simitsidellis I, Gibson DA, Cousins FL, Esnal-Zufiaurre A, Saunders PT. A role for androgens in epithelial proliferation and formation of glands in the mouse uterus. Endocrinology. 2016;157(5):2116-28. Epub 2016 Mar 10. DOI: https://doi.org/10.1210/en.2015-2032
Bracho GS, Altamirano GA, Kass L, Luque EH, Bosquiazzo VL. Hyperandrogenism induces histo-architectural changes in the rat uterus. Reproductive Sciences. 2019;26(5):657-68. Epub 2018 Jun 21. DOI: https://doi.org/10.1177/1933719118783881
Tas M, Kutuk MS, Serin IS, Ozgun MT, Oner G, Ozturk F. Comparison of antiproliferative effects of metformine and progesterone on estrogen-induced endometrial hyperplasia in rats. Gynecological Endocrinology. 2013;29(4):311-4. Epub 2013 Jan 10. DOI: https://doi.org/10.3109/09513590.2012.743010
Virginia AM, Virginia TM, Laura K. Androgen receptor and uterine histoarchitecture in a PCOS rat model. Molecular and Cellular Endocrinology. 2020;518:110973. Epub 2020 Aug 8. DOI: https://doi.org/10.1016/j.mce.2020.110973
Palomba S, Russo T, Orio Jr F, Falbo A, Manguso F, Cascella T, et al. Uterine effects of metformin administration in anovulatory women with polycystic ovary syndrome. Human Reproduction. 2006;21(2):457-65. DOI: https://doi.org/10.1093/humrep/dei351
Lam P, Johnson I, Raine‐Fenning N. Endometrial blood flow is impaired in women with polycystic ovarian syndrome who are clinically hyperandrogenic. Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2009;34(3):326-34. DOI: https://doi.org/10.1002/uog.7314
Adali E, Kolusari A, Adali F, Yildizhan R, Kurdoglu M, Sahin HG. Doppler analysis of uterine perfusion and ovarian stromal blood flow in polycystic ovary syndrome. International Journal of Gynecology & Obstetrics. 2009;105(2):154-7. DOI: https://doi.org/10.1016/j.ijgo.2008.12.023
Xie Y, Xiao L, Li S. Effects of Metformin on Reproductive, Endocrine, and Metabolic Characteristics of Female Offspring in a Rat Model of Letrozole-Induced Polycystic Ovarian Syndrome With Insulin Resistance. Frontiers in Endocrinology. 2021;12. DOI: https://doi.org/10.3389/fendo.2021.701590
Lashen H. Role of metformin in the management of polycystic ovary syndrome. Therapeutic advances in endocrinology and metabolism. 2010;1(3):117-28. DOI: https://doi.org/10.1177/2042018810380215
Stocker T. Climate change 2013: the physical science basis: Working Group I contribution to the Fifth assessment report of the Intergovernmental Panel on Climate Change: Cambridge university press; 2014.
Badawy A, State O, Abdelgawad S. N-Acetyl cysteine and clomiphene citrate for induction of ovulation in polycystic ovary syndrome: a cross-over trial. Acta obstetricia et gynecologica Scandinavica. 2007;86(2):218-22. Erratum in: Acta Obstet Gynecol Scand. 2021 Jun 23. DOI: https://doi.org/10.1080/00016340601090337
Wang L, Tang J, Zhou J, Zhu L, Tan F, Chen Y, et al. N‐Acetyl‐l‐cysteine restores reproductive defects caused by Ggt1 deletion in mice. Clinical and translational medicine. 2021;11(8). DOI: https://doi.org/10.1002/ctm2.510
Furat Rencber S, Kurnaz Ozbek S, Eraldemır C, Sezer Z, Kum T, Ceylan S, et al. Effect of resveratrol and metformin on ovarian reserve and ultrastructure in PCOS: an experimental study. Journal of ovarian research. 2018;11(1):1-16. DOI: https://doi.org/10.1186/s13048-018-0427-7
Mansfield R, Galea R, Brincat M, Hole D, Mason H. Metformin has direct effects on human ovarian steroidogenesis. Fertility and sterility. 2003;79(4):956-62. DOI: https://doi.org/10.1016/S0015-0282(02)04925-7
Maged AM, Elsawah H, Abdelhafez A, Bakry A, Mostafa WA. The adjuvant effect of metformin and N-acetylcysteine to clomiphene citrate in induction of ovulation in patients with Polycystic Ovary Syndrome. Gynecological endocrinology. 2015;31(8):635-8. DOI: https://doi.org/10.3109/09513590.2015.1037269
Chang EY, Barbosa E, Paintlia M, Singh A, Singh I. The use of N-acetylcysteine for the prevention of hypertension in the reduced uterine perfusion pressure model for preeclampsia in Sprague-Dawley rats. American journal of obstetrics and gynecology. 2005;193(3):952-6. DOI: https://doi.org/10.1016/j.ajog.2005.05.083
Salehpour S, Akbari Sene A, Saharkhiz N, Sohrabi MR, Moghimian F. N‐acetylcysteine as an adjuvant to clomiphene citrate for successful induction of ovulation in infertile patients with polycystic ovary syndrome. Journal of Obstetrics and Gynaecology Research. 2012;38(9):1182-6. Epub 2012 Apr 30. DOI: https://doi.org/10.1111/j.1447-0756.2012.01844.x
Ito-Yamaguchi A, Suganuma R, Kumagami A, Hashimoto S, Yoshida-Komiya H, Fujimori K. Effects of metformin on endocrine, metabolic milieus and endometrial expression of androgen receptor in patients with polycystic ovary syndrome. Gynecological Endocrinology. 2015;31(1):44-7. DOI: https://doi.org/10.3109/09513590.2014.951321
Bjørge T, Lukanova A, Jonsson H, Tretli S, Ulmer H, Manjer J, et al. Metabolic syndrome and breast cancer in the me-can (metabolic syndrome and cancer) project. Cancer Epidemiology and Prevention Biomarkers. 2010;19(7):1737-45. DOI: https://doi.org/10.1158/1055-9965.EPI-10-0230
Khalaf WM, Akl SA, Ramadan RR. Effect of Metformin on Endometrial Thickness and Subendometrial Flow Patterns in Anovulatory Patients with Polycystic Ovarian Syndrome. Open Journal of Obstetrics and Gynecology. 2018;8(14):1465. DOI: https://doi.org/10.4236/ojog.2018.814148
Mahamed RR, Maganhin CC, Simões RS, de Jesus Simões M, Baracat EC, Soares Jr JM. Effects of metformin on the reproductive system of androgenized female rats. Fertility and sterility. 2011;95(4):1507-9. DOI: https://doi.org/10.1016/j.fertnstert.2010.07.1093
Elia EM, Belgorosky D, Faut M, Vighi S, Pustovrh C, Motta AB. The effects of metformin on uterine tissue of hyperandrogenized BALB/c mice. Molecular human reproduction. 2009;15(7):421-32. DOI: https://doi.org/10.1093/molehr/gap033
Gao W, Liang J-X, Ma C, Dong J-y, Yan Q. The protective effect of N-acetylcysteine on ionizing radiation induced ovarian failure and loss of ovarian reserve in female mouse. Biomed Research International. 2017;2017. DOI: https://doi.org/10.1155/2017/4176170
Licks F, Hartmann RM, Marques C, Schemitt E, Colares JR, do Couto Soares M, et al. N-acetylcysteine modulates angiogenesis and vasodilation in stomach such as DNA damage in blood of portal hypertensive rats. World Journal of Gastroenterology. 2015;21(43):12351. DOI: https://doi.org/10.3748/wjg.v21.i43.12351
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.


 https://doi.org/10.4081/ejtm.2022.10409
https://doi.org/10.4081/ejtm.2022.10409



