Comparative study between ureter first approach and conventional open Anderson-Hynes pyeloplasty in paediatric patients: A prospective randomised study
Accepted: February 25, 2023
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
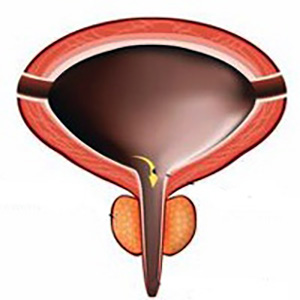
Background: Uretero-pelvic junction obstruction is the most common form of congenital anomaly of the kidney and urinary tract with an incidence of about 1/1.000-1.500 of births and the aetiology and pathogenesis of this anomaly are still unclear until now.
Methods: This is a prospective randomized comparative study conducted from March 2022 to December 2022. Thirty children with uretero-pelvic junction obstruction were included and randomly divided into two groups according to a 1:1 ratio (computer-generated randomization, single blind). Fifteen cases (12 males and 3 female) were subjected to ureter first approach pyeloplasty, and another fifteen (9 males and 6 female) were subjected to conventional Anderson Hynes pyeloplasty.
Results: The mean age of all patients was 6.7 ± 5.4 years in ureter first approach group and 5.1 ± 4.3 years in conventional Anderson-Hynes pyeloplasty group. There were no significant differences between the two groups regarding age, gender, presentation, side, preoperative renogram and post-operative renogram. Also, there were no significant differences between the two groups regarding operative time (in first group 110.3 ± 12.4 and in the second group 111.2 ± 12.0 with p < 0.836), pre and post-operative complication rate. Two cases of urinary tract infections in the first group, one of them having fever, and four cases in the second group, two of them having fever (p < 0.651); four cases of loin pain in the first group and one case in the second group (p < 0.330); one case in the first group having pro- longed leakage of urine for 7 days in post-operative period (p < 0.309). However GFR and t 1⁄2 improved significantly after operation in both groups (p < 0.001).
Conclusions: Ureter first approach is a simple and effective procedure in children with good short term outcomes and could be done safely especially for beginners and less expert surgeons. Finally, it can overcome the problem of long ureteric stricture that may be found intraoperatively because you can shift easily to a flap procedure and complete a tension free anastomosis.
Al Aaraj MS, Badreldin AM. Ureteropelvic Junction Obstruction. 2022 Jul 11. In: StatPearls (Internet). Treasure Island (FL): StatPearls Publishing; 2022.
Klein J, Gonzalez J, Miravete M, et al. Congenital ureteropelvic junction obstruction: human disease and animal models. Int J Exp Pathol. 2011; 92:168-92. DOI: https://doi.org/10.1111/j.1365-2613.2010.00727.x
Chang CP, McDill BW, Neilson JR, et al. Calcineurin is required in urinary tract mesenchyme for the development of the pyeloureter- al peristaltic machinery. J Clin Invest. 2004; 113:1051-8. DOI: https://doi.org/10.1172/JCI20049
Avanoglu A, Tiryaki S. Embryology and Morphological (Mal)Development of UPJ. Front Pediatr. 2020; 8:137. DOI: https://doi.org/10.3389/fped.2020.00137
Ruano-Gil D, Coca-Payeras A, Tejedo-Mateu A. Obstruction and normal recanalization of the ureter in the human embryo. Its rela- tion to congenital ureteric obstruction. Eur Urol. 1975; 1:287-293.
Kajbafzadeh AM, Payabvash S, Salmasi AH, et al. Smooth muscle cell apoptosis and defective neural development in congenital ureteropelvic junction obstruction. J Urol. 2006; 176:718-723. DOI: https://doi.org/10.1016/j.juro.2006.03.041
Wong JC, Rossleigh MA, Farnsworth RH. Utility of technetium- 99m-MAG3 diuretic renography in the neonatal period. J Nucl Med. 1995; 36:2214-9.
Eshima D, Taylor A Jr. Technetium-99m (99mTc) mercap- toacetyltriglycine: update on the new 99mTc renal tubular function agent. Semin Nucl Med. 1992; 22:61-73. DOI: https://doi.org/10.1016/S0001-2998(05)80082-0
Kazlauskas V, Cekuolis A, Bilius V, et al. Diuretic Enhanced Ultrasonography in the Diagnosis of Pyeloureteral Obstruction. Medicina (Kaunas). 2019; 55:670. DOI: https://doi.org/10.3390/medicina55100670
Anderson JC, Hynes W. Plastic operation for hydronephrosis. Proceedings of the Royal Society of Medicine. 1951; 44:4-5. DOI: https://doi.org/10.1177/003591575104400102
Brown T, Mandell J, Lebowitz RL. Neonatal hydronephrosis in the era of sonography. AJR Am J Roentgenol. 1987; 148:959-63. DOI: https://doi.org/10.2214/ajr.148.5.959
Tan BJ, Rastinehad AR, Marcovich R, et al. Trends in uretero- pelvic junction obstruction management among urologists in the United States. Urology. 2005; 65:260-264. DOI: https://doi.org/10.1016/j.urology.2004.09.051
Nayyar R, Kumar P, Panaiyadiyan S, Seth A. Ureter-first Approach and Reduction of Pelvis: Standardizing Handling of Ureteropelvic Junction During Pyeloplasty. Urology. 2022; 160:210- 216. DOI: https://doi.org/10.1016/j.urology.2021.10.030
Dayanc M, Kibar Y, Irkilata HC, et al. A new modification of dis- membered pyeloplasty for primary ureteropelvic junction obstruc- tion. Eur Surg Res. 2008; 40:225-9. DOI: https://doi.org/10.1159/000110865
Diamond DA, Nguyen HT. Dismembered V-flap pyeloplasty. J Urol. 2001; 166:233-235. DOI: https://doi.org/10.1016/S0022-5347(05)66133-2
Salehipour M, Khezri A, Azizi V, Kroup M. Open dismembered tubularized flap pyeloplasty: an effective and simple operation for treatment of ureteropelvic junction obstruction. Urol Int. 2006; 76:345-7. DOI: https://doi.org/10.1159/000092060
Ravish IR, Nerli RB, Reddy MN, Amarkhed SS. Laparoscopic pyeloplasty compared with open pyeloplasty in children. J Endourol. 2007; 21:897-902. DOI: https://doi.org/10.1089/end.2006.0411
Mei H, Pu J, Yang C, et al. Laparoscopic versus open pyeloplas- ty for ureteropelvic junction obstruction in children: a systematic review and meta-analysis. J Endourol. 2011; 25:727-736. DOI: https://doi.org/10.1089/end.2010.0544
Umari P, Lissiani A, Trombetta C, Belgrano E. Comparison of open and laparoscopic pyeloplasty in ureteropelvic junction obstruc- tion surgery: report of 49 cases. Arch Ital Urol Androl. 2011; 83:169-174.
Copyright (c) 2023 the Author(s)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.


 https://doi.org/10.4081/aiua.2023.11231
https://doi.org/10.4081/aiua.2023.11231



