Multiple sclerosis and venous angioplasty for chronic cerebrospinal venous insufficiency: a case control study with ten years follow-up with patients at their own control
Accepted: 16 December 2021
HTML: 5
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Progressive Neurological Diseases (PND) and Chronic Cerebrospinal Venous Insufficiency (CCSVI) and Multiple Sclerosis (MS) have two terms in common: “progressive and chronic” and shortly mean that there is no definitive therapy, at the moment.
The clinical aspects are built on symptoms, upon which the definition of “progression” is based and hence classified. Changement and worsening of symptoms, allow classification of the disease and adjustments are effectively an “up to date” of the disease itself.
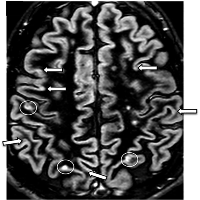
We here resume the ten-year survey of 482 Multiple Sclerosis (MS)-affected patients (314 females, 168 males; mean age =37.8), classified by their Neurology Physicians as Relapse-Remitting (RR), according to the Kurtzke Expanded Disability Status Scale (EDSS), monitoring the parallel presence of CCSVI with clinical MS progression.
Results are present from two homogeneous Relapse-Remitting MS groups of patients divided as “treated and non-treated for CCSVI” with vein angioplasty (vPTA). Furthermore, a Patient’s self-classification based upon symptoms in presence of CCSVI, up to now never implemented, was developed on the basis of both clinical and Duplex vascular issues.
Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald Criteria. Lancet Neurol. 2018;17:162-73. DOI: https://doi.org/10.1016/S1474-4422(17)30470-2
McGinley MP, Goldschmidt CH, Rae-Grant AD. Diagnosis and treatment of multiple sclerosis: a Review. JAMA. 2021;325:765-79. DOI: https://doi.org/10.1001/jama.2020.26858
Katz Sand I. The role of diet in multiple sclerosis: mechanistic connections and current evidence. Curr Nutr Rep. 2018;7:150-60. DOI: https://doi.org/10.1007/s13668-018-0236-z
Saresella M, Mendozzi L, Rossi V, et al. Immunological and clinical effect of diet modulation of the gut microbiome in multiple sclerosis patients: a pilot study. Front Immunol. 2017;8:1391. DOI: https://doi.org/10.3389/fimmu.2017.01391
Parks NE, Jackson-Tarlton CS, Vacchi L, et al. Dietary interventions for multiple sclerosis-related outcomes. Cochrane Database Syst Rev. 2020;5. DOI: https://doi.org/10.1002/14651858.CD004192.pub4
Gell PGH, Coombs, RRA. Classification of allergic reactions responsible for hypersensitivity and disease, p.761-81. In: Gell P, Coombs R, Lachmann P (eds), Clinical Aspects of Immunology. New York, USA, 1975.
Sampson HA. Immunologic mechanisms in adverse reactions to foods. Immunology and Allergy Clinics of North America. 1991;11:701-16. DOI: https://doi.org/10.1016/S0889-8561(22)00070-4
Fulgenzi A, Ferrero ME. EDTA chelation therapy for the treatment of neurotoxicity. Int. J. Mol. Sci. 2019;20:1019. DOI: https://doi.org/10.3390/ijms20051019
Fulgenzi A, Vietti D, Ferrero ME. EDTA chelation therapy in the treatment of neurodegenerative diseases: an update. Biomedicines. 2020;8:269. DOI: https://doi.org/10.3390/biomedicines8080269
Correale J, Gaitán MI, Ysrraelit MC, et al. Progressive multiple sclerosis: from pathogenic mechanisms to treatment. Brain. 2017;140:527-46. DOI: https://doi.org/10.1093/brain/aww258
Spencer JI, Bell JS, DeLuca GC. JVascular pathology in multiple sclerosis: reframing pathogenesis around the blood-brain barrier. Neurol Neurosurg Psychiatry. 2018;89:42-52. DOI: https://doi.org/10.1136/jnnp-2017-316011
Niu J, Tsai HH, Hoi KK, Huang N, et al. Aberrant oligodendroglial-vascular interactions disrupt the blood-brain barrier, triggering CNS inflammation. Nat Neurosci. 2019;22:709-18. DOI: https://doi.org/10.1038/s41593-019-0369-4
Marrie RA, Rudick R, Horwitz R, et al. Vascular comorbidity is associated with more rapid disability progression in multiple sclerosis. Neurology. 2010;74:1041-7. DOI: https://doi.org/10.1212/WNL.0b013e3181d6b125
Geraldes R, Esiri MM, DeLuca GC, Palace J. Age-related small vessel disease: a potential contributor to neurodegeneration in multiple sclerosis. Brain Pathol. 2017;27:707-22. DOI: https://doi.org/10.1111/bpa.12460
Berghoff SA, Duking T, Spieth L, et al. Blood-brain barrier hyperpermeability precedes demyelination in the cuprizone model. Acta Neuropathol Commun. 2017;5:94. DOI: https://doi.org/10.1186/s40478-017-0497-6
Zivadinov R, Weinstock-Guttman B. Extracranial venous angioplasty is ineffective to treat MS. Nature Reviews. Neurology. 2018;14:129-30. DOI: https://doi.org/10.1038/nrneurol.2017.180
Traboulsee AL, Machan L, Girard JM, et al. Safety and efficacy of venoplasty in MS: a randomized, double-blind, sham-controlled phase II trial. Neurology. 2018,30:e1660e1668. DOI: https://doi.org/10.1212/WNL.0000000000006423
Barnett HJM, Plum F, Walton JN. Carotid endarterectomy - an expression of concern. Stroke 1984;15:941-3. DOI: https://doi.org/10.1161/01.STR.15.6.941
Menegatti E, Galeotti R, Gianesini S, et al. Echo-color-Doppler criteria for diagnosis of chronic cerebrospinal venous insufficiency. XVI World Congr UIP 2009. Int Angiol. 2009;28:36.
Lee BB, Bergan J, Gloviczki P, et al. Diagnosis and treatment of venous malformations. Consensus document of the International Union of Phlebology (UIP). Int. Angiol 2009;28:434-51.
Zamboni P, Menegatti E, Weinstock Guttman B, et al. The severity of chronic cerebrospinal venous insufficiency in patients with multiple sclerosis is related to altered cerebrospinal fluid dynamics. Funct Neurol. 2009;24:133-8.
Zamboni P, Galeotti R. The chronic cerebrospinal venous insufficiency syndrome. Phlebology. 2010;25:691-9. DOI: https://doi.org/10.1258/phleb.2010.009083
Simka M, Kostecki J, Zaniewski M, et al. Extracranial Doppler sonographic criteria of chronic cerebrospinal venous insufficiency in the patients with multiple sclerosis. Int Angiol. 2010;29:109-14.
Menegatti E, Genova V, Tessari M, et al. The reproducibility of colour Doppler in chronic cerebrospinal venous insufficiency associated with multiple sclerosis. Int Angiol. 2010;29:121-6.
Laupacis A, Lillie E, Dueck A, et al. Association between chronic cerebrospinal venous insufficiency and multiple sclerosis: a meta-analysis. CMAJ. 2011;183:1203-12. DOI: https://doi.org/10.1503/cmaj.111074
Bavera PM, Mendozzi L, Cavarretta R, Agus GB. Venous extracranial Duplex ultrasound and possible correlations between multiple sclerosis and CCSVI: an observational study after 560 exams. Acta Phlebologica. 2011;12:109-13.
Bavera PM, Agus GB, Alpini D, et al: Results from 823 consecutive duplex exams for CCSVI in a vascular centre. Acta Phlebologica. 2012;13:141-8.
Bavera P. May symptoms of chronic cerebrospinal venous insufficiency be improved by venous angioplasty? Veins and Lymphatics 2015;4:5400. DOI: https://doi.org/10.4081/vl.2015.5400
Zamboni P, Menegatti E, Conforti P, et al. Assessment of cerebral venous return by a novel plethysmography method. J Vasc Surg. 2012;56:677-85. DOI: https://doi.org/10.1016/j.jvs.2012.01.074
Zamboni P, Galeotti R, Salvi F, et al. Effects of venous angioplasty on cerebral lesions in multiple sclerosis: expanded analysis of the Brave Dreams double-blind, sham-controlled randomized trial. J Endovasc Ther. 2020;27:1526602819890110.
Zamboni P, Tesio L, Galimberti S, et al. Efficacy and safety of extracranial vein angioplasty in multiple sclerosis. A randomized clinical trial for the Brave Dreams Research Group. JAMA Neurol. 2018;75:35-43. DOI: https://doi.org/10.1001/jamaneurol.2017.3825
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology.1983;33:1444–52. DOI: https://doi.org/10.1212/WNL.33.11.1444
World Medical Association: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191-4. DOI: https://doi.org/10.1001/jama.2013.281053
Zamboni P, Menegatti E, Cittanti C, et al. Fixing the jugular flow reduces ventricle volume and improves brain perfusion. J Vasc Surg Venous Lymphat Disord. 2016;4:434-45. DOI: https://doi.org/10.1016/j.jvsv.2016.06.006
Messina A, Garofalo G, Faletra A, Piraino D. Three patterns of chronic cerebrospinal venous insufficiency in Ménière syndrome patients: diagnosis and treatment options. Veins and Lymphatics. 2020;9. DOI: https://doi.org/10.4081/vl.2020.8758
Confavreux C, Vukusic S, Moreau T, Adeleine P. Relapses and progression of disability in multiple sclerosis. N Engl J Med. 2000;343:1430-8. DOI: https://doi.org/10.1056/NEJM200011163432001
Piraino D, Garofalo G, Faletra A, Messina A. The omohyoid and sternocleidomastoid muscles entrapment of the internal jugular vein: which role in Mèniére disease patients? Treatment perspective description. Veins and Lymphatics, 2018;7. DOI: https://doi.org/10.4081/vl.2018.7760
Juurlink BHJ, Embry AF, Bavera PM. Reader response: safety and efficacy of venoplasty in MS: a randomized, double-blind, sham-controlled phase II trial. Neurology. 2019;93:319-320. DOI: https://doi.org/10.1212/WNL.0000000000007956
Zamboni P, Galeotti R, Salvi F, et al. Brave Dreams Research Group. Effects of venous angioplasty on cerebral lesions in multiple sclerosis: expanded analysis of the Brave Dreams double-blind, sham-controlled randomized trial. J Endovasc Ther. 2019:1526. DOI: https://doi.org/10.1177/1526602819890110
Giaquinta A, Beggs CB, Veroux M, et al. Factors influencing the hemodynamic response to balloon angioplasty in the treatment of outflow anomalies of internal jugular veins. J Vasc Surg Venous Lymphat Disord. 2017;5:777–88. DOI: https://doi.org/10.1016/j.jvsv.2017.06.015
Napoli V, Berchiolli R, Carboncini MC, et al. Percutaneous venous angioplasty in patients with multiple sclerosis and chronic cerebrospinal venous insufficiency: a randomized wait list control study. Ann Vasc Surg 2020;62:275-86. DOI: https://doi.org/10.1016/j.avsg.2019.05.018
Bavera P. Chronic cerebrospinal venous insufficiency, ten years after. New headlights on a venous disease that enriched the vascular world. Veins and Lymphatics 2020; 9:9053. DOI: https://doi.org/10.4081/vl.2020.9053
Copyright (c) 2021 the Author(s)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/vl.2021.10143
https://doi.org/10.4081/vl.2021.10143




