Prevalence of thyroid dysfunctions in a large, unselected population in Duhok city, Iraqi Kurdistan: A cross-sectional study
Accepted: November 21, 2021
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
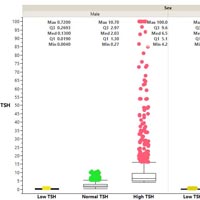
This study aimed to determine the prevalence of Thyroid- Stimulating Hormone (TSH) alterations and different types of thyroid dysfunctions in both sexes with no age limitations from variety of sources in Duhok province. In this retrospective cross-sectional study, we screened 25040 suspicious cases of thyroid diseases in a year (2019), retrieving the data from the computers of three clinical laboratories of Duhok City. Following exclusion of 470 cases, 24568 cases were included to categorize the different types of thyroid dysfunctions. The prevalence of TSH alteration was 25.03%, 20.55% of them had a high concentration being statistically higher in females, while only 4.48% was low TSH with equal prevalence among both sexes. Out of 24568 patients, the prevalence of subclinical hypothyroidism was 94.85%, followed by 2.20%, 1.20%, 0.78%, 0.67%, and 0.31% for each of subclinical hyperthyroidism, primary hypothyroidism, central hyperthyroidism, central hypothyroidism, and primary hyperthyroidism respectively. In conclusion, the studied population had high prevalence of high TSH level (20.55%), being more prevalent in female than in male. Our survey revealed that the distribution of thyroid disorders varied among different age groups with highest prevalence of subclinical hypothyroidism in all age groups (94.85%). We also concluded that middle and advanced ages, and females were more susceptible to thyroid disorders.
Carmona C, Bedoya P, Acevedo J, Arias J. Prevalence of thyroid disorders in an institution providing health services in Medellin-Colombia. Transl Biomed 2018;9:149. DOI: https://doi.org/10.21767/2172-0479.100149
Garmendia Madariaga A, Santos Palacios S, Guillén-Grima F, Galofré JC. The incidence and prevalence of thyroid dysfunction in Europe: a meta-analysis. J Clinical Endocrinol Metab 2014;99:923-31. DOI: https://doi.org/10.1210/jc.2013-2409
Vanderpump MP. The epidemiology of thyroid disease. Br Med Bull 2011;99:39-51. DOI: https://doi.org/10.1093/bmb/ldr030
Bjoro T, Holmen J, Krüger O, et al. Prevalence of thyroid disease, thyroid dysfunction and thyroid peroxidase antibodies in a large, unselected population. The Health Study of Nord-Trondelag (HUNT). Eur J Endocrinol 2000;143:639-47. DOI: https://doi.org/10.1530/eje.0.1430639
Strieder TG, Prummel MF, Tijssen JG, et al. Risk factors for and prevalence of thyroid disorders in a cross‐sectional study among healthy female relatives of patients with autoimmune thyroid disease. Clin Endocrinol 2003;59:396-401. DOI: https://doi.org/10.1046/j.1365-2265.2003.01862.x
Yadav NK, Thanpari C, Shrewastwa MK, et al. Socio demographic wise risk assessment of thyroid function abnormalities in far western region of Nepal: A hospital based descriptive study. Asian Pacific J Trop Dis 2013;3:150-4. DOI: https://doi.org/10.1016/S2222-1808(13)60060-2
Hernandez AG. Principios de bioquímica clínica y patología molecular. Barcelona, Spain Elsevier; 2019.
Cappola AR, Fried LP, Arnold AM, et al. Thyroid status, cardiovascular risk, and mortality in older adults. JAMA 2006;295:1033-41. DOI: https://doi.org/10.1001/jama.295.9.1033
United Nations Children’s Fund. Consumption of iodized salt (% of households) - Iraq The World Bank Website 2019. Available from: https://data.worldbank.org/indicator/SN.ITK.SALT.ZS?end=2018&locations=IQ&start=2018&view=map
Jawzali JI. Regional Differences of Drinking Water Iodine and Its Association with Thyroid Disorder and Serum Iodine. Med J Babylon 2017;14:198-208.
Khattak RM, Ittermann T, Nauck M, et al. Monitoring the prevalence of thyroid disorders in the adult population of Northeast Germany. Population Health Metrics 2016;14:1-11. DOI: https://doi.org/10.1186/s12963-016-0111-3
Nicoloff JT, Spencer CA. The use and misuse of the sensitive thyrotropin assays. J Clin Endocrinol Metab 1990;71:553-8. DOI: https://doi.org/10.1210/jcem-71-3-553
Baloch Z, Carayon P, Conte-Devolx B, et al. Laboratory medicine practice guidelines. Laboratory support for the diagnosis and monitoring of thyroid disease. Thyroid 2003;13:3-126. DOI: https://doi.org/10.1089/105072503321086962
Burtis CA, Bruns DE. Tietz fundamentals of clinical chemistry and molecular diagnostics. e-book. Elsevier Health Sciences; 2014.
Baumgartner C, Da Costa BR, Collet T-H, Feller M, Floriani C, Bauer DC, et al. Thyroid function within the normal range, subclinical hypothyroidism, and the risk of atrial fibrillation. Circulation 2017;136:2100-16. DOI: https://doi.org/10.1161/CIRCULATIONAHA.117.028753
Londoño ÁL, Gallego ML, Bayona A, Landázuri P. Prevalencia de hipotiroidismo y relación con niveles elevados de anticuerpos antiperoxidasa y yoduria en población de 35 y más años en Armenia. 2009-2010. Revista de Salud Pública 2011;13:998-1009. DOI: https://doi.org/10.1590/S0124-00642011000600012
Tunbridge W, Evered D, Hall R, et al. The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol 1977;7:481-93. DOI: https://doi.org/10.1111/j.1365-2265.1977.tb01340.x
Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 2002;87:489-99. DOI: https://doi.org/10.1210/jcem.87.2.8182
Fardella C, Poggi H, Gloger S, et al. Alta prevalencia de enfermedad tiroidea subclínica en sujetos que concurren a control de salud. Revista médica de Chile 2001;129:155-60. DOI: https://doi.org/10.4067/S0034-98872001000200005
Builes CA, Rosero Ó, García J. TSH levels in the evaluation of thryroid disfunction in a population group in Bogota. Acta Médica Colombiana 2006;31:66-70.
Kopp W. Nutrition, evolution and thyroid hormone levels–a link to iodine deficiency disorders? Medical Hypotheses 2004;62:871-5. DOI: https://doi.org/10.1016/j.mehy.2004.02.033
Azizi F. Islamic fasting and thyroid hormones. Intern J Endocrinol Metab 2015;13:e29248. DOI: https://doi.org/10.5812/ijem.13(2)2015.29248
Dubravka B, Ivana G, Nikolina P, et al. The effect of food groups and nutrients on thyroid hormone levels in healthy individuals. Nutrition 2021:111394. DOI: https://doi.org/10.1016/j.nut.2021.111394
Bashar MA, Begam N. Role of dietary factors in thyroid disorders: Current evidences and way forwards. Thyroid Research Practice 2020;17:104. DOI: https://doi.org/10.4103/trp.trp_7_20
Manousou S, Stål M, Larsson C, et al. A Paleolithic-type diet results in iodine deficiency: a 2-year randomized trial in postmenopausal obese women. Eur J Clinical Nutrition 2018;72:124-9. DOI: https://doi.org/10.1038/ejcn.2017.134
Al-Timimi DJ, Mustafa AH. Neonatal screening for congenital hypothyroidism in Duhok Governorate (Iraq); A preliminary study. Duhok Medical J 2019;13:20-30. DOI: https://doi.org/10.31386/dmj.2019.12.1.33
Visser WE, Visser TJ, Peeters RP. Thyroid disorders in older adults. Endocrinol Metab Clin 2013;42:287-303. DOI: https://doi.org/10.1016/j.ecl.2013.02.008
Hasan RI, Raziq AH. Studying the frequency of autoimmune thyroid diseases in Duhok Province. Sci J Univ Zakho 2019;7:45-9. DOI: https://doi.org/10.25271/sjuoz.2019.7.2.587
Qasim BA, Mohammed AA, Ahmed MJ. Lipid profile IN subclinical hypothyroidism: A two centers experience. Duhok Med J 2019;13:56-65. DOI: https://doi.org/10.31386/dmj.2019.13.1.6
Amin ZA, Tawfeeq RD, Kamal SI. The frequency of autoimmune thyroid disorders in patients with thyroid dysfunction in Erbil city. Zanco J Med Sci (Zanco J Med Sci) 2018;22:372-6. DOI: https://doi.org/10.15218/zjms.2018.048
Hamasaeed PA, Hussain SK, Ashraf SM. Evaluation of Thyroid stimulating hormone and thyroid hormone concentrations in females with hypothyroidism and hyperthyroidism. Rafidain J Sci 2019;28:1-7. DOI: https://doi.org/10.33899/rjs.2019.163290
Al Barzanji BAM, Mustafa IH, Aziz KF. Socio-demographic and clinical characteristics of patients with thyroid disorders in Erbil Governorate/Iraq. Diyala J Med 2019;17:28-35. DOI: https://doi.org/10.26505/DJM.17014540225
Khattak KN, Shahmim A, Alam KM, et al. Distribution of thyroid patients between age groups, sex and seasons in the thyroid patients referred to irnum peshawar. J Med Sci 2001;1:400-3. DOI: https://doi.org/10.3923/jms.2001.400.403
Wsoo MA, Rasul KH. Epidemicity of thyroid gland disorders among Ranya Town dwellers: A hospital-based survey. Zanco J Pure Appl Sci 2017;29:1-9. DOI: https://doi.org/10.21271/ZJPAS.29.5.1
Tahir NT, Najim HD, Nsaif AS. Prevalence of overt and subclinical thyroid dysfunction among Iraqi population in Baghdad city. Iraqi J Comm Med 2020;33:20.
Rayman MP. Multiple nutritional factors and thyroid disease, with particular reference to autoimmune thyroid disease. Proceed Nutrition Soc 2019;78:34-44. DOI: https://doi.org/10.1017/S0029665118001192
Huang Y, Cai L, Zheng Y, et al. Association between lifestyle and thyroid dysfunction: A cross-sectional epidemiologic study in the She ethnic minority group of Fujian Province in China. BMC Endocr Disord 2019;19:1-9. DOI: https://doi.org/10.1186/s12902-019-0414-z
Al-Hindawi S, Al-Ghurabi B, andLuaibi N. The role of hla-drb1 allele in hypothyroid patients with and without periodontitis. Pak J Biotechnol 2017;14:629-34.
Vadiveloo T, Donnan PT, Murphy MJ, Leese GP. Age-and gender-specific TSH reference intervals in people with no obvious thyroid disease in Tayside, Scotland: the Thyroid Epidemiology, Audit, and Research Study (TEARS). J Clin Endocrinol Metab 2013;98:1147-53. DOI: https://doi.org/10.1210/jc.2012-3191
Rashad NM, Samir GM. Prevalence, risks, and comorbidity of thyroid dysfunction: a cross-sectional epidemiological study. Egyptian J Int Med 2019;31:635-41.
Otun J, Sahebkar A, Östlundh L, et al. Systematic review and meta-analysis on the effect of soy on thyroid function. Scientific Reports 2019;9:1-9. DOI: https://doi.org/10.1038/s41598-019-40647-x
Bitto A, Polito F, Atteritano M, et al. Genistein aglycone does not affect thyroid function: results from a three-year, randomized, double-blind, placebo-controlled trial. J Clin Endocrinol Metab 2010;95:3067-72. DOI: https://doi.org/10.1210/jc.2009-2779
Marini H, Polito F, Adamo EB, et al. Update on genistein and thyroid: an overall message of safety. Frontiers Endocrinol 2012;3:94. DOI: https://doi.org/10.3389/fendo.2012.00094
Knezevic J, Starchl C, Tmava Berisha A, Amrein K. Thyroid-Gut-Axis: how does the microbiota influence thyroid function? Nutrients 2020;12:1769. DOI: https://doi.org/10.3390/nu12061769
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.


 https://doi.org/10.4081/jbr.2021.10067
https://doi.org/10.4081/jbr.2021.10067



