Effects of inhibition of lymphangiogenesis by the vascular endothelial growth factor receptor 3 (VEGFR-3) inhibitor, MAZ51 on full thickness wounds in mice
Accepted: 22 February 2021
HTML: 58
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
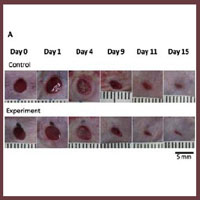
We herein used MAZ51 to inhibit lymphangiogenesis and aimed to clarify the effect of inhibition of lymphangiogenesis on wound healing. BALB/c male mice were divided into two groups: the control group which was injected the dimethyl sulfoxide (DMSO), the experiment group was injected MAZ51 in the DMSO. All wounds were observed for 15 days and the wound areas were measured. Tissue samples were harvested on day 3, 7, 9, 11, 13 and 15, and subjected to immunostaining of blood vessels and lymphatic vessels. There are no significant differences between two groups in the wound area, the number of blood vessels and lymphatic vessels. The number of blood vessels peaked on day 7 in both groups as with previous studies, while the number of lymphatic vessels peaked on 13 or 15 in both groups. This result revealed delayed lymphangiogenesis in comparison with previous studies. The wound healing process in the control and experiment groups were similar, but both groups seemed delayed lymphangiogenesis comparing with previous studies. Injections of MAZ51 or/and DMSO did not affect angiogenesis, while they may affect lymphangiogenesis.
Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res 2009;37:1528-42. DOI: https://doi.org/10.1177/147323000903700531
Kilarski WW. Physiological perspective on therapies of lymphatic vessels. Adv Wound Care (New Rochelle) 2018;7:189-208. DOI: https://doi.org/10.1089/wound.2017.0768
Liao S, von der Weid PY. Inflammation-induced lymphangiogenesis and lymphatic dysfunction. Angiogenesis 2014;17:325-34. DOI: https://doi.org/10.1007/s10456-014-9416-7
Singh AV, Gemmati D, Kanase A, et al. Nanobiomaterials for vascularbiology and wound manage-ment: A review. Veins and Lymphatics 2018;7:7196. DOI: https://doi.org/10.4081/vl.2018.7196
Singh AV, Subhashree L, Milani P, et al. Interplay of iron metallobiology, metalloproteinases, and FXIII, and role of their gene variants in venous leg ulcer. Int J Low Extrem Wounds 2010;9:166-79. DOI: https://doi.org/10.1177/1534734610384653
Komatsu E, Nakajima Y, Mukai K, et al. Lymph drainage during wound healing in a hindlimb lymphedema mouse model. Lymphat Res Biol 2017;15:32-8. DOI: https://doi.org/10.1089/lrb.2016.0026
Kirkin V, Mazitschek R, Krishnan J, et al. Characterization of indolinones which preferentially inhibit VEGF-C- and VEGF-D-induced activation of VEGFR-3 rather than VEGFR-2. Eur J Biochem 2001;268:5530-40. DOI: https://doi.org/10.1046/j.1432-1033.2001.02476.x
Kirkin V, Thiele W, Baumann P, et al. MAZ51, an indolinone that inhibits endothelial cell and tumor cell growth in vitro, suppresses tumor growth in vivo. Int J Cancer 2004;112:986-93. DOI: https://doi.org/10.1002/ijc.20509
Takahashi N, Itoh MT, Ishizuka B. Human chorionic gonadotropin induces nestin expression in endothelial cells of the ovary via vascular endothelial growth factor signaling. Endocrinology 2008;149:253-60. DOI: https://doi.org/10.1210/en.2007-0774
Dwivedi C, Pandey I, Pandey H, et al. In vivo diabetic wound healing with nanofibrous scaffolds modified with gentamicin and recombinant human epidermal growth factor. J Biomed Mater Res Part A 2018;106A:641-51. DOI: https://doi.org/10.1002/jbm.a.36268
Dwivedi C, Pandey H, Pandey AC, et al. In vivo biocompatibility of electrospun biodegradable dual carrier (antibiotic + growth factor) in a mouse model-implications for rapid wound healing. Pharmaceutics 2019;11:180. DOI: https://doi.org/10.3390/pharmaceutics11040180
Shimamura K, Nakatani T, Ueda A, et al. Relationship between lymphangiogenesis and exudates during the wound-healing process of mouse skin full-thickness wound. Wound Repair Regen 2009;17:598-605. DOI: https://doi.org/10.1111/j.1524-475X.2009.00512.x
Mawaki A, Nakatani T, Sugama J, Konya C. Relationship between the distribution of myofibroblasts, and stellar and circular scar formation due to the contraction of square and circular wound healing. Anat Sci Int 2007;82:147-55. DOI: https://doi.org/10.1111/j.1447-073X.2007.00179.x
Tanaka A, Nakatani T, Sugama J, et al. Histological examination of the distribution change of myofibroblasts in the wound contraction. EWMA Jour 2004;4:13-8.
Paavonen K, Puolakkainen P, Jussila L, et al. Vascular endothelial growth factor receptor-3 in lymphangiogenesis in wound healing. Am J Pathol 2000;156:1499-504. DOI: https://doi.org/10.1016/S0002-9440(10)65021-3
Cao Y. Direct role of PDGF-BB in lymphangiogenesis and lymphatic metastasis. Cell Cycle 2005;4:228-30. DOI: https://doi.org/10.4161/cc.4.2.1421
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/vl.2021.9385
https://doi.org/10.4081/vl.2021.9385




