Prospects of plasmapheresis for patients with severe COVID-19
Accepted: 2 September 2020
HTML: 7
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
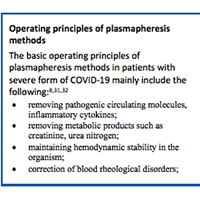
On February 11, 2020, the World Health Organization officially named the infection caused by the new coronavirus “Coronavirus disease 2019” (COVID-19). On February 11, 2020, the International Committee on Taxonomy of Viruses (ICTV) officially named the infectious matter “severe acute respiratory syndrome coronavirus 2” (SARS-CoV-2). Emergence of severe complications with new coronavirus disease is due to the development of hypercytokinaemia, also known as “cytokine storm”. These complications comprise acute respiratory distress syndrome (ARDS), respiratory failure and death. Emerging data point to the logic of using extracorporeal haemocorrection to normalise cytokine levels and reduce the severity of organ disorders. The analysis of the literature indicates that to date, a certain positive experience has been accumulated in the world in the application of extracorporeal methods in clinical practice in patients with COVID-19.
Ma J, Xia P, Zhou Y, Liu Z, Zhou X, Wang J, Li T, Yan X, Chen L, Zhang S, Qin Y, Li X. Potential effect of blood purification therapy in reducing cytokine storm as a late complication of critically ill COVID-19. Clin Immunol. 2020 Apr 1;214:108408. doi: 10.1016/j.clim.2020.108408. DOI: https://doi.org/10.1016/j.clim.2020.108408
Chen C, Zhang XR, Ju ZY, He WF. Advances in the research of cytokine storm mechanism induced by Corona Virus Disease 2019 and the corresponding immunotherapies. Zhonghua Shao Shang Za Zhi. 2020 Mar 1;36(0):E005. doi: 10.3760/cma.j.cn501120-20200224-00088.
Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, Tan KS, Wang DY, Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020 Mar 13;7(1):11. doi: 10.1186/s40779-020-00240-0. Review. DOI: https://doi.org/10.1186/s40779-020-00240-0
Liu Y, Zhang C, Huang F, Yang Y, Wang F, Yuan J, et al. 2019-novel coronavirus (2019-nCoV) infections trigger an exaggerated cytokine response aggravating lung injury. 2020.
Chaolin Huang, Yeming Wang, Xingwang Li, Prof, Lili Ren, Jianping Zhao, Yi Hu, Li Zhang, Guohui Fan, Jiuyang Xu, Xiaoying Gu, Zhenshun Cheng, Ting Yu, Jiaan Xia, Yuan Wei, Wenjuan Wu, Xuelei Xie, Wen Yin, Hui Li, Min Liu, Yan Xiao, Hong Gao, Li Guo, Jungang Xie, Guangfa Wang, Rongmeng Jiang, Zhancheng Gao, Qi Jin, Jianwei Wang, and Bin Cao. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 15-21 February; 395(10223): 497–506. doi: 10.1016/S0140-6736(20)30183-5. DOI: https://doi.org/10.1016/S0140-6736(20)30183-5
Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J. COVID-19: consider cytokine storm syndrome and immunosuppresion. Lancet. 2020;395(10229):1033–1034. DOI: https://doi.org/10.1016/S0140-6736(20)30628-0
Tabibi S, Tabibi T, Conic RRZ, Banisaeed N, Streiff MB. Therapeutic Plasma Exchange: A potential Management Strategy for Critically Ill COVID-19 Patients. J Intensive Care Med. 2020 Sep;35(9):827-835. DOI: https://doi.org/10.1177/0885066620940259
Xiang-Hong Yang, Ren-Hua Sun, Ming-Yan Zhao, Er-Zhen Chen, Jiao Liu, Hong-Liang Wang, Rong-Li Yang, and De-Chang Chenc. Expert recommendations on blood purification treatment protocol for patients with severe COVID-19. Chronic Dis Transl Med. 2020 Apr 28. DOI: https://doi.org/10.1016/j.cdtm.2020.04.002
Keith P, Day M, Perkins L, Moyer L, Hewitt K, Wells A. A novel treatment approach to the novel coronavirus: an argument for the use of therapeutic plasma exchange for fulminant COVID-19. Crit Care. 2020 Apr 2;24(1):128. doi: 10.1186/s13054-020-2836-4. DOI: https://doi.org/10.1186/s13054-020-2836-4
Avdeev SN. Acute respiratory distissue syndrome. Consilium medicum. 2005. V. 7, No. 4. - Pp. 330-338. (in russ.)
Pourahmad R, Moazzami B, Rezaei N. Efficacy of Plasmapheresis and Immunoglobulin Replacement Therapy (IVIG) on Patients with COVID-19.SN Compr Clin Med. 2020 Jul 31:1-5. doi: 10.1007/s42399-020-00438-2. DOI: https://doi.org/10.1007/s42399-020-00438-2
Kalinin NN. Clinical application of extracorporeal treatment methods. Publishing House: Trackpore Technology CJSC, 2006, P. 168. (in russ.)
Ragimov AA, Poreshina SA, Salimov EL. Plasmapheresis in systemic inflammatory response at P14. М.: Journal “Practical medicine”, 2008. 124 Pp. (in russ.). Illustrated.
Madore F. Plasmapheresis. Technical aspects and indications. Crit Care Clin. 2002;18(2):375–92.
Hirano R, Namazuda K, Hirata N. Double filtration plasmapheresis: Review of current clinical applications. Ther Apher Dial. 2020 Jun 19. doi: 10.1111/1744-9987.13548. DOI: https://doi.org/10.1111/1744-9987.13548
Navarro-Martínez R, Cauli O. Therapeutic Plasmapheresis with Albumin Replacement in Alzheimer's Disease and Chronic Progressive Multiple Sclerosis: A Review. Pharmaceuticals (Basel). 2020 Feb 12;13(2):28. DOI: https://doi.org/10.3390/ph13020028
Sergent SR, Ashurst JV. Plasmapheresis. 2020 Jul 15. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan.
Schwartz J, Padmanabhan A, Aqui N, Balogun RA, Connelly-Smith L, Delaney M, Dunbar NM, Witt V, Wu Y, Shaz BH. Guidelines on the Use of Therapeutic Apheresis in Clinical Practice-Evidence-Based Approach from the Writing Committee of the American Society for Apheresis: The Seventh Special Issue. J Clin Apher. 2016 Jun;31(3):149-62. DOI: https://doi.org/10.1002/jca.21470
Clark WF, Huang SS. Introduction to therapeutic plasma exchange. Transfus Apher Sci. 2019 Jun;58(3):228-229. doi: 10.1016/j.transci.2019.04.004. Epub 2019 Apr 26. DOI: https://doi.org/10.1016/j.transci.2019.04.004
Sokolov AA, Popov AV. Cascade plasmofiltration: method characteristic and equipment selection. Tverskoi meditsinskii zhurnal. 2017. No. 5. Pp. 46-58. (in russ.)
Sokolov AA, Tishko VV, Belskikh AN, Esipov AV. Modern extracorporal technologies: prospects of use. Gospital'naya medicina: nauka i praktika. 2019. V. 1. No. 1. Pp. 32-41. (in russ.)22. Соколов А.А., Попов А.В. Каскадная плазмофильтрация: характеристика метода, выбор оборудования. Тверской медицинский журнал. 2017. № 5. С. 46-58.
Rubtsov MS, Shukevich DL. Modern extracorporeal methods for critical conditions caused by systemic inflammatory response (review). Anesteziologiya i reanimatologiya. 2019;(4): 20-30. (in russ.) doi: 10.17116/anaesthesiology201904120 DOI: https://doi.org/10.17116/anaesthesiology201904120
ShenC, WangZ, ZhaoF, YangY, LiJ, YuanJ, WangF, LiD, YangM, XingL, WeiJ, XiaoH, YangY, QuJ, QingL, ChenL, XuZ, PengL, LiY, ZhengH, ChenF, HuangK, JiangY, LiuD, ZhangZ, LiuY, LiuL. Treatmentof 5 CriticallyIllPatientsWithCOVID-19 WithConvalescentPlasma. JAMA. 2020 Mar 27. doi: 10.1001/jama.2020.4783. DOI: https://doi.org/10.1001/jama.2020.4783
Bloch EM, Shoham S, Casadevall A, Sachais BS, Shaz B, Winters JL, van Buskirk C, Grossman BJ, Joyner M, Henderson JP, Pekosz A, Lau B, Wesolowski A, Katz L, Shan H, Auwaerter PG, Thomas D, Sullivan DJ, Paneth N, Gehrie E, Spitalnik S, Hod E, Pollack L, Nicholson WT, Pirofski LA, Bailey JA, Tobian AA. Deployment of convalescent plasma for the prevention and treatment of COVID-19. J Clin Invest. 2020 Apr 7. pii: 138745. doi: 10.1172/JCI138745. DOI: https://doi.org/10.1172/JCI138745
Chen L, Xiong J, Bao L, Shi Y. Convalescent plasma as a potential therapy for COVID-19. Lancet Infect Dis. 2020 Apr;20(4):398-400. doi: 10.1016/S1473-3099(20)30141-9. Epub 2020 Feb 27. DOI: https://doi.org/10.1016/S1473-3099(20)30141-9
Murphy M, Estcourt L, Grant-Casey J, Dzik S. International Survey of Trials of Convalescent Plasma to Treat COVID-19 Infection. Transfus Med Rev. 2020 Jun 27:S0887-7963(20)30031-6.
Rajendran K, Narayanasamy K, Rangarajan J, Rathinam J, Natarajan M, Ramachandran A. Convalescent plasma transfusion for the treatment of COVID-19: Systematic review. J Med Virol. 2020 May 1. doi: 10.1002/jmv.25961. DOI: https://doi.org/10.1002/jmv.25961
J Seghatchian, and F Lanza. Convalescent Plasma, an Apheresis Research Project Targeting and Motivating the Fully Recovered COVID 19 Patients: A Rousing Message of Clinical Benefit To Both Donors and Recipients Alike. Transfus Apher Sci. 2020 Apr 23 : 102794. DOI: https://doi.org/10.1016/j.transci.2020.102794
Wei Cao and Taisheng Li. COVID-19: towards understanding of pathogenesis. Cell Res. 2020 Apr 28 : 1–3. DOI: https://doi.org/10.1038/s41422-020-0327-4
Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia.J Thromb Haemost. 2020 Apr; 18(4):844-847. DOI: https://doi.org/10.1111/jth.14768
Sloan Steven R., Andrzejewski Chester, Aqui Nicole A., Kiss Joseph E., Krause Peter J., Park Yara A. Role of therapeutic apheresis in infectious and inflammatory diseases: Current knowledge and unanswered questions. Journal of Clinical Apheresis. 2014;30(5):259–264. doi: 10.1002/jca.21370. DOI: https://doi.org/10.1002/jca.21370
Yang XH, Sun RH, Zhao MY, Chen EZ, Liu J, Wang HL, Yang RL, Chen DC. Expert recommendations on blood purification treatment protocol for patients with severe COVID-19: Recommendation and consensus. Chronic Dis Transl Med. 2020 Apr 28. doi: 10.1016/j.cdtm.2020.04.002. DOI: https://doi.org/10.1016/j.cdtm.2020.04.002
Keith P, Wells A, Hodges J, et al. The therapeutic efficacy of adjunct therapeutic plasma exchange for septic shock with multiple organ failure: a single center retrospective review. 2020. Preprint at https://www.researchsquare.com/article/rs-16022/v1. DOI: https://doi.org/10.21203/rs.3.rs-16022/v2
Shi H., Zhou C., He P., Huang S., Duan Y., Wang X. Successful treatment of plasma exchange followed by intravenous immunogloblin in a critically ill patient with 2019 novel coronavirus infection. Int J Antimicrob Agents. 2020:105974. DOI: https://doi.org/10.1016/j.ijantimicag.2020.105974
Central Board of the Scientific Society of Experts of Extracorporeal Blood Treatment in Intensive Care. Interim recommendations on the use of methods of extracorporeal haemocorrection in the complex treatment of patients with new coronavirus disease COVID-19.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.


 https://doi.org/10.4081/ejtm.2020.9165
https://doi.org/10.4081/ejtm.2020.9165



