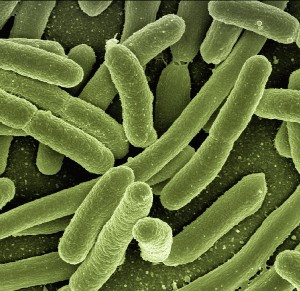
Antibacterial and antibiofilm effects of gold and silver nanoparticles against the uropathogenic Escherichia coli by scanning electron microscopy (SEM) analysis
Accepted: 18 October 2023
HTML: 5
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Uropathogenic Escherichia coli (UPEC) is a nosocomial pathogen associated with urinary tract infections and biofilm formation, which contributes to antibiotic resistance. Discovering potent antibacterial agents is crucial. This study aimed to assess the antibacterial and antibiofilm effects of gold and silver nanoparticles on UPEC using Scanning Electron Microscopy (SEM). UPEC biofilms were cultivated on nitrocellulose membranes for 48 hours at 37°C, then treated with gold nanoparticles (50 ppm and 100 ppm) and silver nanoparticles (50 ppm and 100 ppm) for another 48 hours. Antibacterial and antibiofilm activities were evaluated through cell density and SEM analysis. SEM revealed lower cell density, reduced biofilm formation, and altered cell morphology with rough, wrinkled surfaces after nanoparticle treatment. In conclusion, gold and silver nanoparticles exhibit antibacterial and antibiofilm properties, as observed in SEM analysis. SEM is a valuable tool for studying the antimicrobial effects of nano gold and silver on bacterial cell morphology and biofilm populations.
Sari YIP, Rohmah UN, Andini SA, Luwao HP. Summary of the Prevention of Catheter-Associated Urinary Tract Infection in An Intensive Care Unit. Jurnal Ners 2019;14:103–7. DOI: https://doi.org/10.20473/jn.v14i3.17010
Javed S, Mirani ZA, Pirzada ZA. Phylogenetic Group B2 Expressed Significant Biofilm Formation among Drug Resistant Uropathogenic Escherichia coli. Libyan J Med 2021;16:1845444. DOI: https://doi.org/10.1080/19932820.2020.1845444
Issa OM, Bakir WAE, Abbas MA. Laboratory diagnosis of urinary tract infections in patients with resistance genes towards antibiotics. Bionatura 2022;7:46. DOI: https://doi.org/10.21931/RB/2022.07.02.46
Sjahriani T, Wasito EB, Tyasningsih W. Isolation and Identification of Escherichia coli O157:H7 Lytic Bacteriophage from Environment Sewage. Int J Food Sci 2021;2021:7383121. DOI: https://doi.org/10.1155/2021/7383121
Katongole P, Nalubega F, Florence NC, et al. Biofilm formation, antimicrobial susceptibility and virulence genes of Uropathogenic Escherichia coli isolated from clinical isolates in Uganda. BMC Infect Dis 2020;20:1–6. DOI: https://doi.org/10.1186/s12879-020-05186-1
Syaiful I, Widodo ADW, Endraswari PD, et al. The association between biofilm formation abilitand antibiotic resistance phenotype in clinical isolates of gram-negative bacteria: a cross-sectional study. Bali Med J 2023;12:1014–20.
Boya BR, Lee JH, Lee J. Antibiofilm and Antimicrobial Activities of Chloroindoles Against Uropathogenic Escherichia coli. Front Microbiol 2022;13:872943. DOI: https://doi.org/10.3389/fmicb.2022.872943
Magtoto R, Poonsuk K, Baum D, et al. Evaluation of the Serologic Cross-Reactivity between Transmissible Gastroenteritis Coronavirus and Porcine Respiratory Coronavirus Using Commercial Blocking Enzyme-Linked Immunosorbent Assay Kits. mSphere 2019;4:e00017-19. DOI: https://doi.org/10.1128/mSphere.00017-19
Bharadwaj KK, Rabha B, Choudhury BK, et al. Current strategies in inhibiting biofilm formation for combating urinary tract infections: Special focus on peptides, nano-particles and phytochemicals. Biocatal Agricult Biotechnol 2021;38:102209. DOI: https://doi.org/10.1016/j.bcab.2021.102209
Yang YM, Osawa K, Kitagawa K, et al. Differential effects of chromosome and plasmid blaCTX-M-15 genes on antibiotic susceptibilities in extended-spectrum beta-lactamase-producing Escherichia coli isolates from patients with urinary tract infection. Int J Urol 2021;28:623–8. DOI: https://doi.org/10.1111/iju.14498
Sonawane JM, Rai AK, Sharma M, et al. Microbial biofilms: Recent advances and progress in environmental bioremediation. Sci Total Environ 2022;824:153843. DOI: https://doi.org/10.1016/j.scitotenv.2022.153843
Olar R, Badea M, Chifiriuc MC. Metal Complexes-A Promising Approach to Target Biofilm Associated Infections. Molecules 2022;27:758. DOI: https://doi.org/10.3390/molecules27030758
Mhawesh A, Khudair M, Abbas ON. Major Genetic Determinants of Extended-Spectrum β-Lactamase (ESBL), Carbapenemase, Fosfomycin and Colistin Resistance in Escherichia Coli from Intensive Care Units. Bionatura. 2022;7:11. DOI: https://doi.org/10.21931/RB/2022.07.01.11
Waskito LA, Yamaoka Y. The Story of Helicobacter pylori: Depicting Human Migrations from the Phylogeography. Adv Exp Med Biol 2019;1149:1-16. DOI: https://doi.org/10.1007/5584_2019_356
Eleraky NE, Allam A, Hassan SB, Omar MM. Nanomedicine Fight against Antibacterial Resistance: An Overview of the Recent Pharmaceutical Innovations. Pharmaceutics 2020;12:142. DOI: https://doi.org/10.3390/pharmaceutics12020142
Zubair N, Akhtar K. Morphology controlled synthesis of ZnO nanoparticles for in-vitro evaluation of antibacterial activity. Trans Nonferrous Metals Soc China 2020;30:1605–14. DOI: https://doi.org/10.1016/S1003-6326(20)65323-7
Sathiyaraj S, Suriyakala G, Dhanesh Gandhi A, et al. Biosynthesis, characterization, and antibacterial activity of gold nanoparticles. J Infect Public Health 2021;14:1842–7. DOI: https://doi.org/10.1016/j.jiph.2021.10.007
Shah R, Shah SA, Shah S, Faisal S, Ullah AF. Green synthesis and antibacterial activity of gold nanoparticles of digera muricata. Indian J Pharmaceut Sci 2020;82:374–8. DOI: https://doi.org/10.36468/pharmaceutical-sciences.659
Allafchian A, Vahabi MR, Jalali SAH, et al. Design of green silver nanoparticles mediated by Ferula ovina Boiss. Extract with enhanced antibacterial effect. Chem Physics Lett 2022;791:139392. DOI: https://doi.org/10.1016/j.cplett.2022.139392
Swidan NS, Hashem YA, Elkhatib WF, Yassien MA. Antibiofilm activity of green synthesized silver nanoparticles against biofilm associated enterococcal urinary pathogens. Sci Rep 2022;12:3869. DOI: https://doi.org/10.1038/s41598-022-07831-y
Seo M, Oh T, Bae S. Antibiofilm activity of silver nanoparticles against biofilm forming Staphylococcus pseudintermedius isolated from dogs with otitis externa. Vet Med Sci 2021;7:1551–7. DOI: https://doi.org/10.1002/vms3.554
Rusu D, Stratul SI, Calniceanu H, et al. A qualitative and semiquantitative SEM study of the morphology of the biofilm on root surfaces of human teeth with endodontic-periodontal lesions. Experim Therapeutic Med 2020;20:201. DOI: https://doi.org/10.3892/etm.2020.9331
Kitagawa K, Shigemura K, Yamamichi F, et al. International Comparison of Causative Bacteria and Antimicrobial Susceptibilities of Urinary Tract Infections between Kobe, Japan, and Surabaya, Indonesia. Jpn J Infect Dis 2018;71:8–13. DOI: https://doi.org/10.7883/yoken.JJID.2017.233
Purbowati R, Sugiharto, Listyawati AF, et al. Antibacterial and antibiofilm effect of silver and gold nanoparticles in Uropathogenic Escherichia coli. Berkala Penelitian Hayati 2021;27(2 SE-Articles). DOI: https://doi.org/10.23869/bphjbr.27.2.20222
Alhamid MZ, Hadi BS, Khumaeni A. Synthesis of silver nanoparticles using laser ablation method utilizing Nd:YAG laser. AIP Conf Proceed 2019;2202:20013. DOI: https://doi.org/10.1063/1.5141626
Jailani A, Ahmed B, Lee JH, Lee J. Inhibition of Agrobacterium tumefaciens Growth and Biofilm Formation by Tannic Acid. Biomedicines 2022;10:1619. DOI: https://doi.org/10.3390/biomedicines10071619
Ibrahim H. Nanotechnology and Its Applications to Medicine: an over view. QJM Int J Med 2020;113:hcaa060.008. DOI: https://doi.org/10.1093/qjmed/hcaa060.008
Mutalik C, Lin IH, Krisnawati DI, et al. Antibacterial Pathways in Transition Metal-Based Nanocomposites: A Mechanistic Overview. Int J Nanomed 2022;17:6821–42. DOI: https://doi.org/10.2147/IJN.S392081
Wang S, Gao Y, Jin Q, Ji J. Emerging antibacterial nanomedicine for enhanced antibiotic therapy. Biomat Sci 2020;8(:6825–39. DOI: https://doi.org/10.1039/D0BM00974A
Garg P, Attri P, Sharma R, et al. Advances and Perspective on Antimicrobial Nanomaterials for Biomedical Applications. Front Nanotechnol 2022:4. DOI: https://doi.org/10.3389/fnano.2022.898411
Balachandar R, Navaneethan R, Biruntha M, et al. Antibacterial activity of silver nanoparticles phytosynthesized from Glochidion candolleanum leaves. Materials Letters 2022;311:131572. DOI: https://doi.org/10.1016/j.matlet.2021.131572
Alarjani KM, Huessien D, Rasheed RA, Kalaiyarasi M. Green synthesis of silver nanoparticles by Pisum sativum L. (pea) pod against multidrug resistant foodborne pathogens. J King Saud University - Sci 2022;34:101897. DOI: https://doi.org/10.1016/j.jksus.2022.101897
Hashemi Z, Shirzadi-Ahodashti M, Mortazavi-Derazkola S, Ebrahimzadeh MA. Sustainable biosynthesis of metallic silver nanoparticles using barberry phenolic extract: Optimization and evaluation of photocatalytic, in vitro cytotoxicity, and antibacterial activities against multidrug-resistant bacteria. Inorg Chem Comm 2022;139. DOI: https://doi.org/10.1016/j.inoche.2022.109320
Gouyau J, Duval RE, Boudier A, Lamouroux E. Investigation of Nanoparticle Metallic Core Antibacterial Activity: Gold and Silver Nanoparticles against Escherichia coli and Staphylococcus aureus. Int J Mol Sci 2021;22:1905. DOI: https://doi.org/10.3390/ijms22041905
Mobed A, Hasanzadeh M, Shadjou N, et al. Immobilization of ssDNA on the surface of silver nanoparticles-graphene quantum dots modified by gold nanoparticles towards biosensing of microorganism. Microchem J 2020;152:104286. DOI: https://doi.org/10.1016/j.microc.2019.104286
Miškovská A, Rabochová M, Michailidu J, et al. Antibiofilm activity of silver nanoparticles biosynthesized using viticultural waste. PLoS One 2022;17:e0272844. DOI: https://doi.org/10.1371/journal.pone.0272844
Siddique MH, Aslam B, Imran M, et al. Effect of Silver Nanoparticles on Biofilm Formation and EPS Production of Multidrug-Resistant Klebsiella pneumoniae. BioMed Res Int 2020;2020:6398165. DOI: https://doi.org/10.1155/2020/6398165
Kong AS, Maran S, Yap PS, et al. Anti- and Pro-Oxidant Properties of Essential Oils against Antimicrobial Resistance. Antioxidants (Basel) 2022;11:1819. DOI: https://doi.org/10.3390/antiox11091819
De Silva C, Nawawi NM, Karim MMA, et al. The mechanistic action of biosynthesised silver nanoparticles and its application in aquaculture and livestock industries. Animals (Basel) 2021;11:2097. DOI: https://doi.org/10.3390/ani11072097
Mathelié-Guinlet M, Asmar AT, Collet JF, Dufrêne YF. Lipoprotein Lpp regulates the mechanical properties of the E. coli cell envelope. Nature Comm 2020;11:1789. DOI: https://doi.org/10.1038/s41467-020-15489-1
Ali SG, Ansari MA, Alzohairy MA, et al. Biogenic Gold Nanoparticles as Potent Antibacterial and Antibiofilm Nano-Antibiotics against Pseudomonas aeruginosa. Antibiotics (Basel) 2020;9:100. DOI: https://doi.org/10.3390/antibiotics9030100
Gómez-Núñez MF, Castillo-López M, Sevilla-Castillo F, et al. Nanoparticle-Based Devices in the Control of Antibiotic Resistant Bacteria. Front Microbiol 2020;11:563821. DOI: https://doi.org/10.3389/fmicb.2020.563821
Ali S, Perveen S, Ali M, et al. Bioinspired morphology-controlled silver nanoparticles for antimicrobial application. Mat Sci Engin C 2020;108:110421. DOI: https://doi.org/10.1016/j.msec.2019.110421
Rodríguez-Serrano C, Guzmán-Moreno J, Ángeles-Chávez C, et al. Biosynthesis of silver nanoparticles by Fusarium scirpi and its potential as antimicrobial agent against uropathogenic Escherichia coli biofilms. PLoS One 2020;15:e0230275. DOI: https://doi.org/10.1371/journal.pone.0230275
Funari R, Shen AQ. Detection and Characterization of Bacterial Biofilms and Biofilm-Based Sensors. ACS Sensors 2022;7:347–57. DOI: https://doi.org/10.1021/acssensors.1c02722
Algabar FAA, Baqer BA. Detection of biofilm formation of (Serratia and E.coli ) and determination of the inhibitory effect of Quercus plant extract against these infectious pathogens. Bionatura 2022;7:8. DOI: https://doi.org/10.21931/RB/2022.07.01.8
Copyright (c) 2023 the Author(s)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.


 https://doi.org/10.4081/hls.2023.11748
https://doi.org/10.4081/hls.2023.11748



