Fibrin sealants in lumbar annuloplasty after endoscopic discectomy as a method to prevent recurrent lumbar disc herniation
Accepted: 24 January 2020
HTML: 51
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
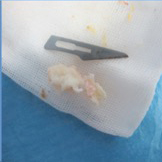
Fibrin sealant as a promising agent for providing scaffold and efficient hemostasis is widely accepted in several specialties. However, the outcome of Fibrin sealants in lumbar annuloplasty after endoscopic discectomy has not been evaluated in patients with disc herniation. The goal of this study was to evaluate the efficacy, response, and probability of future recurrence rates in herniated nucleus pulposus (HNP) with the use of fibrin sealant in conjunction with endoscopic disc surgery. A total of 35 patients (28 men, 7women) were evaluated, including 18 patients who underwent endoscopic discectomy alone and 17 patients that received fibrin sealant at the site of annulus tear and endoscopic discectomy. All patients were followed through both clinical and imaging methods for an average of 10.5 months. Primary outcome measure was defined as lumbar decompression approved by imaging and symptom alleviation after endoscopic spinal discectomy with Visual Analogue Scale (VAS) score ≤ 4 (cut-off point). Median size of annular tearing was significantly lower in the endoscopic discectomy group (median, 3) (minimum, 2; maximum, 5); however, the corresponding factor in the endoscopic discectomy plus fibrin sealant group was significantly larger (median, 6) (minimum, 5; maximum, 10), with P <0.001. Only one patient in the endoscopic discectomy group had an HNP recurrence during follow-up compared to two patients in the endoscopic discectomy plus fibrin sealant group. Due to the temporary effects of fibrin sealant in preventing disc herniation and the observed recurrence rate in both the case and control groups, the results of this study suggest a role of fibrin sealants combined with endoscopic discectomy to prevent early HNP recurrence rate.
Weber H. Lumbar disc herniation: a controlled, prospective study with ten years of observation. Spine. 1983;8(2):131-40. DOI: https://doi.org/10.1097/00007632-198303000-00003
Deyo RA, Tsui-Wu Y-J. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine. 1987;12(3):264-8. DOI: https://doi.org/10.1097/00007632-198704000-00013
Ahn Y, Lee S-H. Outcome predictors of percutaneous endoscopic lumbar discectomy and thermal annuloplasty for discogenic low back pain. Acta neurochirurgica. 2010;152(10):1695-702. DOI: https://doi.org/10.1007/s00701-010-0726-2
CHOY DS. Percutaneous laser disc decompression (PLDD): twelve years' experience with 752 procedures in 518 patients. Journal of clinical laser medicine & surgery. 1998;16(6):325-31. DOI: https://doi.org/10.1089/clm.1998.16.325
Aizawa T, Ozawa H, Kusakabe T, Tanaka Y, Sekiguchi A, Hashimoto K, et al. Reoperation rates after fenestration for lumbar spinal canal stenosis: a 20-year period survival function method analysis. European Spine Journal. 2015;24(2):381-7. DOI: https://doi.org/10.1007/s00586-014-3479-4
Tsou PM, Yeung CA, Yeung AT. Posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain: a minimal access visualized intradiscal surgical procedure. The Spine Journal. 2004;4(5):564-73. DOI: https://doi.org/10.1016/j.spinee.2004.01.014
Lee S-H, Kang HS. Percutaneous endoscopic laser annuloplasty for discogenic low back pain. World neurosurgery. 2010;73(3):198-206. DOI: https://doi.org/10.1016/j.surneu.2009.01.023
Esposito F, Angileri FF, Kruse P, Cavallo LM, Solari D, Esposito V, et al. Fibrin sealants in dura sealing: a systematic literature review. PloS one. 2016;11(4):e0151533. DOI: https://doi.org/10.1371/journal.pone.0151533
Epstein NE. A review article on the benefits of early mobilization following spinal surgery and other medical/surgical procedures. Surgical neurology international. 2014;5(Suppl 3):S66. DOI: https://doi.org/10.4103/2152-7806.130674
Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best practice & research Clinical rheumatology. 2010;24(6):769-81. DOI: https://doi.org/10.1016/j.berh.2010.10.002
Medzhitov R. Origin and physiological roles of inflammation. Nature. 2008;454(7203):428-35. DOI: https://doi.org/10.1038/nature07201
Molinos M, Almeida CR, Caldeira J, Cunha C, Gonçalves RM, Barbosa MA. Inflammation in intervertebral disc degeneration and regeneration. Journal of The Royal Society Interface. 2015;12(104):20141191. DOI: https://doi.org/10.1098/rsif.2014.1191
Risbud MV, Shapiro IM. Role of cytokines in intervertebral disc degeneration: pain and disc content. Nature Reviews Rheumatology. 2014;10(1):44-56. DOI: https://doi.org/10.1038/nrrheum.2013.160
Takahashi H, Suguro T, Okazima Y, Motegi M, Okada Y, Kakiuchi T. Inflammatory cytokines in the herniated disc of the lumbar spine. Spine. 1996;21(2):218-24. DOI: https://doi.org/10.1097/00007632-199601150-00011
Peterson CK, Pfirrmann CW, Hodler J, Leemann S, Schmid C, Anklin B, et al. Symptomatic, Magnetic Resonance Imaging–Confirmed Cervical Disk Herniation Patients: A Comparative-Effectiveness Prospective Observational Study of 2 Age-and Sex-Matched Cohorts Treated With Either Imaging-Guided Indirect Cervical Nerve Root Injections or Spinal Manipulative Therapy. Journal of manipulative and physiological therapeutics. 2016;39(3):210-7. DOI: https://doi.org/10.1016/j.jmpt.2016.02.004
Lee JH, Lee S-H. Clinical and radiological characteristics of lumbosacral lateral disc herniation in comparison with those of medial disc herniation. Medicine. 2016;95(7). DOI: https://doi.org/10.1097/MD.0000000000002733
Tidrick R, Warner E. Fibrin fixation of skin transplants. Surgery. 1944;15(1):90-5.
Panda A, Kumar S, Kumar A, Bansal R, Bhartiya S. Fibrin glue in ophthalmology. Indian Journal of ophthalmology. 2009;57(5):371. DOI: https://doi.org/10.4103/0301-4738.55079
Kirilak Y, Pavlos NJ, Willers CR, Han R, Feng H, Xu J, et al. Fibrin sealant promotes migration and proliferation of human articular chondrocytes: possible involvement of thrombin and protease-activated receptors. International journal of molecular medicine. 2006;17(4):551-8. DOI: https://doi.org/10.3892/ijmm.17.4.551
Dickneite G, Metzner H, Pfeifer T, Kroez M, Witzke G. A comparison of fibrin sealants in relation to their in vitro and in vivo properties. Thrombosis research. 2003;112(1):73-82. DOI: https://doi.org/10.1016/j.thromres.2003.10.010
Thompson DF, Letassy NA, Thompson GD. Fibrin glue: a review of its preparation, efficacy, and adverse effects as a topical hemostat. Drug intelligence & clinical pharmacy. 1988;22(12):946-52. DOI: https://doi.org/10.1177/106002808802201203
Isogai N, Landis WJ, Mori R, Gotoh Y, Gerstenfeld LC, Upton J, et al. Experimental use of fibrin glue to induce site-directed osteogenesis from cultured periosteal cells. Plastic and reconstructive surgery. 2000;105(3):953-63. DOI: https://doi.org/10.1097/00006534-200003000-00019
Polo-Corrales L, Latorre-Esteves M, Ramirez-Vick JE. Scaffold design for bone regeneration. Journal of nanoscience and nanotechnology. 2014;14(1):15-56. DOI: https://doi.org/10.1166/jnn.2014.9127
Moore WR, Graves SE, Bain GI. Synthetic bone graft substitutes. ANZ journal of surgery. 2001;71(6):354-61. DOI: https://doi.org/10.1046/j.1440-1622.2001.02128.x
Lee O, Coathup M, Goodship A, Blunn G. Use of mesenchymal stem cells to facilitate bone regeneration in normal and chemotherapy-treated rats. Tissue engineering. 2005;11(11-12):1727-35. DOI: https://doi.org/10.1089/ten.2005.11.1727
Abiraman S, Varma H, Umashankar P, John A. Fibrin glue as an osteoinductive protein in a mouse model. Biomaterials. 2002;23(14):3023-31. DOI: https://doi.org/10.1016/S0142-9612(02)00064-9
Tayapongsak P, O'Brien DA, Monteiro CB, Arceo-Diaz LY. Autologous fibrin adhesive in mandibular reconstruction with particulate cancellous bone and marrow. Journal of oral and maxillofacial surgery. 1994;52(2):161-5. DOI: https://doi.org/10.1016/0278-2391(94)90401-4
Class L, Burri C, Gerngross H, Mutschler W. Bone healing stimulated by plasma Factor XIII: Osteotomy experiments in sheep. Acta orthopaedica Scandinavica. 1985;56(1):57-62. DOI: https://doi.org/10.3109/17453678508992981
Ito K, Yamada Y, Naiki T, Ueda M. Simultaneous implant placement and bone regeneration around dental implants using tissue‐engineered bone with fibrin glue, mesenchymal stem cells and platelet‐rich plasma. Clinical oral implants research. 2006;17(5):579-86. DOI: https://doi.org/10.1111/j.1600-0501.2006.01246.x
Giannini G, Mauro V, Agostino T, Gianfranco B. Use of autologous fibrin-platelet glue and bone fragments in maxillofacial surgery. Transfusion and apheresis science. 2004;30(2):139-44. DOI: https://doi.org/10.1016/j.transci.2003.11.009
Wiltse LL, Berger PE, McCulloch JA. A system for reporting the size and location of lesions in the spine. Spine. 1997;22(13):1534-7. DOI: https://doi.org/10.1097/00007632-199707010-00023
Kovac D. Automated endoscopic percutaneous diskectomy in the treatment of lumbar disk hernia. Lijecnicki vjesnik. 1991;113(5-6):158-61.
Mayer H, Brock M, Berlien H-P, Weber B. Percutaneous Endoscopic Laser Discectomy (PELD) A New Surgical Technique for Non-sequestrated Lumbar Discs. Minimally Invasive Neurosurgery I: Springer; 1992. p. 53-8. DOI: https://doi.org/10.1007/978-3-7091-6687-1_7
Birkenmaier C, Komp M, Leu HF, Wegener B, Ruetten S. The current state of endoscopic disc surgery: review of controlled studies comparing full-endoscopic procedures for disc herniations to standard procedures. Pain Physician. 2013;16(4):335-44. DOI: https://doi.org/10.36076/ppj.2013/16/335
Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic anterior decompression versus conventional anterior decompression and fusion in cervical disc herniations. International orthopaedics. 2009;33(6):1677. DOI: https://doi.org/10.1007/s00264-008-0684-y
Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine. 2008;33(9):931-9. DOI: https://doi.org/10.1097/BRS.0b013e31816c8af7
Hou T, Zhou Q, Dai F, Luo F, He Q, Zhang J, et al. Repeated microendoscopic discectomy for recurrent lumbar disk herniation. Clinics. 2015;70(2):120-5. DOI: https://doi.org/10.6061/clinics/2015(02)09
Jordan JL, Konstantinou K, O'Dowd J. Herniated lumbar disc. BMJ clinical evidence. 2011;2011.
Choi G, Lee S-H, Raiturker PP, Lee S, Chae Y-S. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5–S1 using a rigid working channel endoscope. Operative Neurosurgery. 2006;58(suppl_1):ONS-59-ONS-68. DOI: https://doi.org/10.1227/01.NEU.0000192713.95921.4A
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejtm.2020.8748
https://doi.org/10.4081/ejtm.2020.8748



