Clinical manifestation and microbial profiling of recurrent MDR microorganisms associated with head and neck infection- a retrospective study
Accepted: 28 July 2023
HTML: 3
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
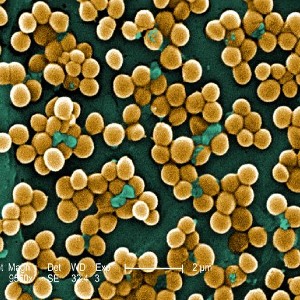
Head and neck infection (HNI) can lead to life-threatening complications, including death. The purpose of this study is to look at the entire clinico-demographic profile of patients with HNI as well as the microbiologic profile of recurring bacterial infection cases with a variety of symptoms. A retrospective cross-sectional study was conducted on 1080 HNI patients in a tertiary care hospital in Bhubaneswar, Odisha, India, from January 2018 to December 2022. Of the 1080 cases, 771 (71.39%) were males, 309 (28.61%) were females, and 603 (55.83%) were from rural areas reporting to a tertiary care hospital. 62% of the cases were between the ages of 31 and 60. Neck abscesses account for 570 (52.78%) of all cases, with parotid abscesses accounting for 233 (21.57%), peritonsillar abscesses accounting for 170 (15.74%), otitis media 32 (2.96%), and oral cavity infection accounting for 26 (2.41%). In 854 (79.07%) cases, the etiology was odontogenic, followed by sinus in 188 (17.41%) and otogenic in 38 (3.52%). The most common presenting features were neck swelling in 537 (49.72%) cases and face swelling in 238 (22.04%) cases, followed by jaw pain in 26 (2.41%) cases and others. Patients were hospitalized for an average of 11.824.38 days. Treatment and recurrence had a strong significant relationship (p 0.001). Microbiologic investigation of recurrent patients revealed 12 microorganisms, including bacteria and fungus, mainly multidrug-resistant in given ascending order Staphylococcus aureus (26.74%), Klebsiella pneumoniae, Pseudomonas aeruginosa, Acinetobacter baumannii, Escherichia coli, Candida albicans (4.65%), Aspergillus fumigatus, A. flavus, A. niger, C. tropicalis, C. glabrata, C. krusei. Apart from colistin, almost all antibiotics were highly resistant to gram-negative bacteria, whereas against S. aureus, benzylpenicillin, and oxacillin showed 100% resistance, followed by erythromycin (91.3%), levofloxacin (86.96%), and ciprofloxacin (82.61%). This exploratory study would aid in determining the HNI burden and epidemiology, as well as their treatment status.
Duarte MJ, Ket al Reinshagen K, Knoll RM, Abdullah KG, Welling DB, Jung DH. Otogenic brain abscesses A systematic review. Laryngoscope Investigative Otolaryngol 2018;3:198-208. DOI: https://doi.org/10.1002/lio2.150
Brożek-Mądryz E, Waniewska-Łęczycka M, Robert B, Krzeski A. Head, and neck abscesses in complicated acute otitis Media-Pathways and classification. Otolaryngol (Sunnyvale) 2018;8:2.
Pucci R, Cassoni A, Di Carlo D, et al. Odontogenic-Related Head, and Neck Infections: From Abscess to Mediastinitis: Our Experience, Limits, and Perspectives—A 5-Year Survey. Int J Environ Res Public Health 2023;20:3469. DOI: https://doi.org/10.3390/ijerph20043469
Fan X, Peters BA, Jacobs EJ, et al. Drinking alcohol is associated with variation in the human oral microbiome in a large study of American adults. Microbiome 2018;6:1-5. DOI: https://doi.org/10.1186/s40168-018-0448-x
Hidaka H, Yamaguchi T, Hasegawa J, et al.Clinical and bacteriological influence of diabetes mellitus on deep neck infection: systematic review and meta‐analysis. Head Neck 2015;37:1536-1546. DOI: https://doi.org/10.1002/hed.23776
Juncar M, Popa AR, Baciuţ MF, et al. Evolution assessment of head and neck infections in diabetic patients–A case-control study. J Craniomaxillofac Surg 2014;42:498-502. DOI: https://doi.org/10.1016/j.jcms.2013.06.009
Gonzalez-Beicos A. Nunez D. Imaging of acute head and neck infections. Radiologic Clinics 2012;50:73-83. DOI: https://doi.org/10.1016/j.rcl.2011.08.004
Velhonoja J, Lääveri M, Soukka T, Irjala H, Kinnunen I. Deep neck space infections: an upward trend and changing characteristics. Eur Arch Oto-Rhino-Laryngol 2020;277:863-872. DOI: https://doi.org/10.1007/s00405-019-05742-9
Bali RK, Sharma P, Gaba S, et al. A review of complications of odontogenic infections. Nat J Maxillofac Surg 2015;6:136. DOI: https://doi.org/10.4103/0975-5950.183867
Boscolo-Rizzo P, Stellin M, Muzzi E, et al. Deep neck infections: a study of 365 cases highlighting recommendations for management and treatment. Eur Arch Oto-Rhino-Laryngol 2012;269:1241-1249. DOI: https://doi.org/10.1007/s00405-011-1761-1
Walia IS, Borle RM, Mehendiratta D, Yadav AO. Microbiology and antibiotic sensitivity of head and neck space infections of odontogenic origin. J Maxillofac Oral Sur 2014;13:16-21. DOI: https://doi.org/10.1007/s12663-012-0455-6
CDC Summary health statistics: national health interview survey. 2016 Accessed June 18, 2018. Available from: https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2016_SHS_Table_A-2.pdf
Cramer JD, Purkey MR, Smith SS, Schroeder Jr JW. The impact of delayed surgical drainage of deep neck abscesses in adult and pediatric populations. Laryngoscope 2016;126:1753-1760. DOI: https://doi.org/10.1002/lary.25835
Seneviratne S, Hoffman G, Varadhan H, et al. Does microbial colonization of a neck drain predispose to surgical site infection: clean vs clean-contaminated procedures. Eur Arch Oto-Rhino-Laryngol 2018;275:1249-1255. DOI: https://doi.org/10.1007/s00405-018-4921-8
Šámal V, Paldus V, Fáčková D, et al. The prevalence of antibiotic-resistant and multidrug-resistant bacteria in urine cultures from inpatients with spinal cord injuries and disorders: an 8-year, single-centre study. BMC Infect Dis 2022;22:1-1. DOI: https://doi.org/10.1186/s12879-022-07235-3
Becerra MC, Appleton SC, Franke MF, et al. Recurrence after treatment for pulmonary multidrug-resistant tuberculosis. Clininfects Dis 2010;51:709-11. DOI: https://doi.org/10.1086/655892
Horcajada JP, Montero M, Oliver A, et al. Epidemiology and treatment of multidrug-resistant and extensively drug-resistant Pseudomonas aeruginosa infections. Clin Microbiol Rev 2019;32:e00031-19. DOI: https://doi.org/10.1128/CMR.00031-19
Moon J, Yoon CH, Kim MK, Oh JY. The incidence and outcomes of recurrence of infection after therapeutic penetrating keratoplasty for medically-uncontrolled infectious keratitis. J Clin Med 2020;9:3696. DOI: https://doi.org/10.3390/jcm9113696
Dudhe P, Burse K, Kulkarni S, et al. Clinical Profile and Outcome of Head and Neck Abscesses in 68 Patients at a Tertiary Care Centre. Ind J Otolaryngol Head Neck Surg 2022;29:1-7. DOI: https://doi.org/10.1007/s12070-022-03409-2
Kataria G, Saxena A, Bhagat S, Singh B, Kaur M, Kaur G. Deep neck space infections: a study of 76 cases. Iran J Otorhinolaryngol 2015;27:293.
Brożek-Mądryz E, Waniewska-Łęczycka M, Robert B, Krzeski A. Head and Neck Abscesses in Complicated Acute Otitis Media-Pathways and Classification. Otolaryngol (Sunnyvale) 2018;8:2. DOI: https://doi.org/10.4172/2161-119X.1000345
Marioni G, Staffieri A, Parisi S, et al. Rational diagnostic and therapeutic management of deep neck infections: analysis of 233 consecutive cases. Ann Otol Rhinol Laryngol 2010;119:181-187. DOI: https://doi.org/10.1177/000348941011900306
Grisaru-Soen G, Komisar O, Aizenstein O, Soudack M, Schwartz D, Paret G. Retropharyngeal and parapharyngeal abscess in children—epidemiology, clinical features, and treatment. Int J Pedia Otorhinolaryngol 2010;74:1016-1020. DOI: https://doi.org/10.1016/j.ijporl.2010.05.030
Chang L, Chi H, Chiu NC, et al. Deep neck infections in different age groups of children. J Microbiol Immunol Infect 2010;43:47-52. DOI: https://doi.org/10.1016/S1684-1182(10)60007-2
Carbone PN, Capra GG, Brigger MT. Antibiotic therapy for pediatric deep neck abscesses a systematic review. Int J Pedia Otorhinolaryngol 2012;76:1647-53. DOI: https://doi.org/10.1016/j.ijporl.2012.07.038
Nathoo N, Nadvi SS, NarotamPK, van Dellen JR. Brain abscess: management and outcome analysis of a computed tomography era experience with 973 patients. World Neurosurg 2011;75:716-726. DOI: https://doi.org/10.1016/j.wneu.2010.11.043
Nusbaum AO, Som PM, Rothschild MA, Shugar JM. Recurrence of a deep neck infection: a clinical indication of an underlying congenital lesion. Arch Otolaryngol Head Neck Surg 1999;125:1379-82. DOI: https://doi.org/10.1001/archotol.125.12.1379
Das AK, Venkatesh MD, Gupta SC, Kashyap RC. Recurrent deep neck space infections. Med J Arm Forc Ind 2013;59:349-50. DOI: https://doi.org/10.1016/S0377-1237(03)80155-7
Chen MY, Lo YC, Chen WC, Wang KF, Chan PC. Recurrence after successful treatment of multidrug-resistant tuberculosis in Taiwan. PloS One 2017;12:e0170980. DOI: https://doi.org/10.1371/journal.pone.0170980
Holland SM, Gallin JI. Evaluation of the patient with recurrent bacterial infections. Annu Rev Med 1998;49:185-99. DOI: https://doi.org/10.1146/annurev.med.49.1.185
Yu J, Jiang F, Zhang F, et al.Thermonucleases contribute to Staphylococcus aureus biofilm formation in implant-associated infections–a redundant and complementary story. Front Microbiol 2021;12:687888. DOI: https://doi.org/10.3389/fmicb.2021.687888
Goering RV, Swartzendruber EA, Obradovich AE, et al. The emergence of oxacillin resistance in stealth methicillin-resistant Staphylococcus aureus due to mecA sequence instability. Antimicrob Agents Chemother 2019;63:e00558-19. DOI: https://doi.org/10.1128/AAC.00558-19
Kampf G, Adena S, Rüden H, Weist K. Inducibility and potential role of mecA-gene-positive oxacillin-susceptible Staphylococcus aureus from colonized healthcare workers as a source for nosocomial infections. J Hosp Inf 2013;54:124-9. DOI: https://doi.org/10.1016/S0195-6701(03)00119-1
Penn C, Moddrell C, Tickler IA, Henthorne MA, Kehrli M, Goering RVet al. Wound infections caused by inducible methicillin-resistant Staphylococcus aureus strains. J Glob Antimicrob Resist 2013;1:79-83. DOI: https://doi.org/10.1016/j.jgar.2013.03.009
Bearman GM, Rosato AE, Assanasen S, et al. Nasal carriage of inducible dormant and community-associated methicillin-resistant Staphylococcus aureus in an ambulatory population of predominantly university students. Int J Infect Dis 2010;14:e18-24.h DOI: https://doi.org/10.1016/j.ijid.2009.09.005
Copyright (c) 2023 the Author(s)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.


 https://doi.org/10.4081/hls.2023.11527
https://doi.org/10.4081/hls.2023.11527



