A rare case report of post-Covid Mucormycosis-Aspergillosis co-infection
HTML: 11
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Background and Purpose:
Mucormycosis and Aspergillosis square measure the foremost frequent fungal infections caused by these filiform fungi. Coinfection is scarce and incorporates a poor prognosis. The commonest presentation of invasive fungal infection (IFI) is rhinocerebral involvement. It ordinarily affects immunocompromised patients.
Case report:
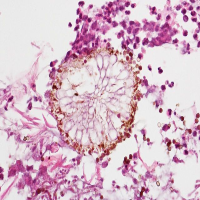
A 55-year-old post-COVID male patient with uncontrolled Diabetes Mellitus developed swelling and chemosis in the left eye. In plain CT orbit, mucosal thickenings were seen in the ethmoid, sphenoid, left frontal, and left maxillary sinuses without any erosions or extensions. Nasal endoscopy showed black-brown overgrowth on the left middle turbinate. Biopsy revealed growth of both Mucor and Aspergillus. The patient was treated for Diabetic Ketoacidosis along with Amphotericin-B for anti-fungal management and showed significant improvement and is stable.
Conclusion:
It is probably the first rare case of coinfection with Mucormycosis (Rhizopus spp.) and Aspergillosis (Aspergillus flavus). Early diagnosis is a major advantage in management. The multidisciplinary approach of such cases is invaluable. The implementation of higher diagnostic methods including PCR in the diagnosis at all tertiary care facilities. A refined selection of post-COVID cases in higher numbers and cautious collection and processing of patient specimens will certainly attribute to higher chances of a definitive diagnosis and an early initiation of specific and efficient treatment.
Afroze SN, Korlepara R, Rao GV, Madala J. Mucormycosis in a diabetic patient: a case report with an insight into its pathophysiology. Contemp Clin Dent. 2017;8:662-666. DOI: https://doi.org/10.4103/ccd.ccd_558_17
Artis WM, Fountain JA, Delcher HK, Jones HE. A mechanism of susceptibility to Mucormycosis in diabetic ketoacidosis: transferrin and iron availability. Diabetes. 1982;31:1109-14. DOI: https://doi.org/10.2337/diabetes.31.12.1109
Castrejon-Perez A, Welsh EC, Miranda I, et al. Cutaneous Mucormycosis. Bras Dermatol. 2017;92:304-11. DOI: https://doi.org/10.1590/abd1806-4841.20176614
Goel S, Palaskar S, Shetty VP, Bhushan A. Rhinomaxillary Mucormycosis with cerebral extension. J Oral Maxillofac Pathol. 2009;13:14-7. DOI: https://doi.org/10.4103/0973-029X.48743
Kajs-Wyllie M. Hyperbaric oxygen therapy for rhinocerebral fungal infection. J Neurosci Nurs. 1995;27:174-81. DOI: https://doi.org/10.1097/01376517-199506000-00006
Kosmidis C, Denning DW. The clinical spectrum of pulmonary aspergillosis. Thorax. 2015;70:270-7. DOI: https://doi.org/10.1136/thoraxjnl-2014-206291
Lador N, Polacheck I, Gural A, et al. A trifungal infection of the mandible: case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:451-6. DOI: https://doi.org/10.1016/j.tripleo.2005.07.022
In: Marx RE, Stern D (eds.), Inflammatory, reactive and infectious diseases in oral and maxillofacial pathology, p.104-6. 2003, Quintessence Publishing, Carol Stream III, USA.
Mehta S, Pandey A. Rhino-orbital Mucormycosis associated with COVID-19. Cureus. 2020;12: e10726. DOI: https://doi.org/10.7759/cureus.10726
Neville WB, Damm D, Allen CM, Bouquot JE. Textbook of oral & maxillofacial pathology, 2nd ed. 2001, Philadelphia, USA. 768 pp.
Petrikkos G, Skiada A, Lortholary O, et al. Epidemiology and clinical manifestations of Mucormycosis. Clin Infect Dis. 2012;54:S23–S34. DOI: https://doi.org/10.1093/cid/cir866
Roden MM, Zaoutis TE, Buchanan WL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41:634-653. DOI: https://doi.org/10.1086/432579
Salisbury PL, Caloss R, Cruz JM, et al. Mucormycosis of the mandible after dental extractions in a patient with acute myelogenous leukemia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:340-4. DOI: https://doi.org/10.1016/S1079-2104(97)90240-7
Spellberg B, Walsh TJ, Kontoyiannis DP, et al. Recent advances in the management of Mucormycosis: from bench to bedside. Clin Infect Dis. 2009;48:1743-51. DOI: https://doi.org/10.1086/599105
Torres-Narbona M, Guinea J, Muñoz P, Bouza E. Zygomycetes and zygomycosis in the new era of antifungal therapies. Rev Esp Quimioter. 2007;20:375-86.
Viterbo S, Fasolis M, Garzino-Demo P, et al. Management and outcomes of three cases of rhinocerebral Mucormycosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:e69-74. DOI: https://doi.org/10.1016/j.tripleo.2011.04.048
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/mm.2021.9918
https://doi.org/10.4081/mm.2021.9918



