Dermatophytic infection and in vitro activities of antifungal drugs against dermatophytes in rural India
Accepted: 26 October 2021
HTML: 6
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Background
Increase in resistance to conventional antifungals renders the need for antifungal sensitivity testing in Dermatophytes.
The present study aimed at determining the prevalence of dermatophytic infections and their susceptibility pattern in a rural healthcare facility.
Methods
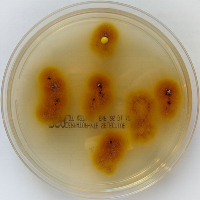
Patients with suspected dermatophytosis attending the dermatology outpatient department were enrolled in the study. Specimen collection for mycological examinations was done. In-vitro antifungal sensitivity testing was performed as per the Clinical and Laboratory Standard Institute (CLSI) M38-A2 (2008) standards with broth microdilution method.
Results
Onychomycosis was the commonest (41.9%) presentation. Dermatophytic prevalence based on culture was 110 (70.9%). The commonest species was Trichophyton rubrum (36.8%). Terbinafine was found to be the most effective drug, followed by ketoconazole and itraconazole.
Conclusion
Antifungal sensitivity in dermatophytic infections should be made a routine in tertiary healthcare facilities as we are already witnessing the rampage of emerging fungal infection– Mucormycosis in the nation and worldwide.
Andrews JM. Determination of minimum inhibitory concentrations. J Antimicrob Chemother. 2001;48:5-16 DOI: https://doi.org/10.1093/jac/48.suppl_1.5
Amod Yadav K, Urhekar AD, Mane V, et al. Optimization and isolation of dermatophytes from clinical samples and in vitro antifungal susceptibility testing by disc diffusion method. Journal of Microbiol and Biotechn 2013; E-ISSN 2320-3528.
Bhatia VK, Sharma PC. Determination of minimum inhibitory concentrations of itraconazole, terbinafine and ketoconazole against dermatophyte species by broth microdilution method. Indian J Med Microbiol. 2015;33:533-7. DOI: https://doi.org/10.4103/0255-0857.167341
Chander J. Textbook of medical mycology: dermatophytosis. 4th edition. New Delhi, India: Jaypee publishing; 2018. 40 pp.
Doddamani PV, Harshan KH, Kanta RC, et al. Isolation, identification and prevalence of dermatophytes in tertiary care hospital in Gulbarga district. People’s Journal of Scientific Research. 2013;6:10-13.
Fernández-Torres B, Carrillo AJ, Martín E, et al. In vitro activities of 10 antifungal drugs against 508 dermatophyte strains. Antimicrob Agents Chemother 2001;45:2524-8. DOI: https://doi.org/10.1128/AAC.45.9.2524-2528.2001
Ghannoum MA, Chaturvedi V, Espinel-Ingroff A, et al. Intra- and inter-laboratory study of a method for testing the antifungal susceptibilities of dermatophytes. J Clin Microbiol 2004;42:2977-9. DOI: https://doi.org/10.1128/JCM.42.7.2977-2979.2004
Goldstein AO, Smith KM, Ives TJ, Goldstein B. Mycotic infection. Effective management of condition involving skin, hair and nails. Geriatrics 2000;55:40-2,45-7,51-2.
Grover S, Roy P. Clinico-mycological profile of superficial mycosis in a hospital in North-East India. MJAFI 2003;59:114-116. DOI: https://doi.org/10.1016/S0377-1237(03)80053-9
Gupta S, Agrawal P, Rajawat R, Gupta S. Prevalence of dermatophytic infection and determining sensitivity of diagnostic procedures. Int J Pharm Sci. 2014;6:35-38.
Jessup CJ, Warner J, Isham N, et al. Antifungal susceptibility testing of dermatophytes: establishing a medium for inducing conidial growth and evaluation of susceptibility of clinical isolates J Clin Microbiol. 2000;38:341-4. DOI: https://doi.org/10.1128/JCM.38.1.341-344.2000
Kumar Y, Singh K, Kanodia S, et al. Clinico-epidemological profile of superficial fungal infections in Rajasthan. MedPulse-IntMed J 2015;2:139-43.
Lakshmanan A, Ganeshkumar P, Mohan SR, et al. Epidemiological and clinical pattern of dermatomycoses in rural India. Indian J Med Microbiol. 2015;33:134-6. DOI: https://doi.org/10.4103/0255-0857.150922
Lavanya V, Solabannavar SS. Clinico-mycological study of dermatophytosis in a tertiary care center in Bagalkot. Int J Med 2015;1:63-66.
Mahajan S, Tilak R, Kaushal SK, et al. Clinico-mycological study of dermatophytic infections and their sensitivity to antifungal drugs in a tertiary care center. Indian J Dermatol Venereol Leprol. 2017;83:436-40. DOI: https://doi.org/10.4103/ijdvl.IJDVL_519_16
Manjunath M, Koppad M, Dadapeer S. Clinico-mycological study of dermatomycosis in a tertiary care hospital. Indian J Microbiol Res. 2016;3:190-193. DOI: https://doi.org/10.5958/2394-5478.2016.00043.1
Mishra M, Mishra S, Singh PC, Mishra BC. Clinico-mycological profile of superficial mycoses. Indian J Dermatol Venerol Leprol 1998:64:283-5.
Penmetcha U, Myneni RB, Yarlagadda P, Simgamsetty S. A study of prevalence of dermatophytosis in and around Guntur District, Andhra Pradesh, South India. Int J Curr Microbiol App Sci. 2016;5:702-17. DOI: https://doi.org/10.20546/ijcmas.2016.509.081
Perea S, Fothergill AW, Sutton DA, Rinaldi MG. Comparison of in vitro activities of voriconazole and five established antifungal agents against different species of dermatophytes using a broth macrodilution method. J Clin Microbiol. 2001;39:385-8. DOI: https://doi.org/10.1128/JCM.39.1.385-388.2001
Suman S, Beena M. Profile of dermatophyte infections in Baroda. Indian J Dermatol and Venereol 2003;69:281-283.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/mm.2021.9917
https://doi.org/10.4081/mm.2021.9917



