Assessment of potential factors that support the endemicity of cholera in Nigeria from food handlers, health workers and the environment
Potential factors that support the endemicity of cholera in Nigeria
Accepted: 27 October 2021
HTML: 12
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
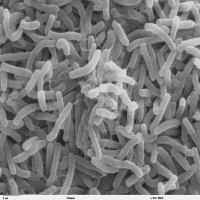
Background and Aims: Diarrheal diseases caused by bacterial pathogens are widespread and they result in morbidity and mortality of a lot of people yearly. The aim of this study was to assess the role of the environment, health workers and food handlers as reservoirs of Vibrio cholerae, and other diarrhea causing bacteria. Methods: Healthcare workers were proportionally selected and multistage sampling technique was adopted in selecting food handlers for the study. A total of 374 participants consisting of health workers and food handlers were recruited. Socio-demographic and clinical information were collected using questionnaires, while stool and environmental samples were also collected. Results: More female 55.9 % than male 44.1 % participated in the study and the mean age of participants was 38.7 ± 10.9. A significant number of participants identified poor hygiene practices as the major cause of diarrhea. V. cholerae O1 serotype was not detected in any of the environmental samples nor stool samples of both food handlers and health workers. However, V. cholerae (Non O1/Non O139) was isolated from the stool samples of food handlers and health workers in Kano State implying that they could be serving a source of the continuous dissemination of the pathogen. Other bacterial pathogens that are aetiology of diarrhea including Salmonella spp. Escherichia coli, Klebsiella oxytoca, and Enterobacter spp. were also isolated. Conclusion: It is therefore imperative that food handlers and health workers undergo periodic health checks to ensure they are free of pathogens they could easily transmit through food or to patients.
Ajayi A, Smith SI. Recurrent cholera epidemics in Africa: which way forward? A literature review. Infect. 2018;47:341-349. DOI: https://doi.org/10.1007/s15010-018-1186-5
Akabanda F, Hlortsi EH, Owusu-Kwarteng J. Food safety knowledge, attitudes and practices of institutional food-handlers in Ghana. BMC Public Health. 2017;17:40. DOI: https://doi.org/10.1186/s12889-016-3986-9
Akoachere J-F T K, Masalla TN, Njom HA. Multidrug resistant toxigenic Vibrio cholerae O1 is persistent in water sources in New Bell-Douala, Cameroon. BMC Infect Dis. 2013;13:66. DOI: https://doi.org/10.1186/1471-2334-13-366
Ali M, Lopez AL, You YA, et al. The global burden of cholera. Bull World Health Organ. 2012;90:209-18A. DOI: https://doi.org/10.2471/BLT.11.093427
Amoo OS, Smith SI, Ujah IA, et al. Socio economic and health challenges of internally-displaced persons as a result of 2012 flooding in Nigeria. Ceylon J Sci. 2018;47:229-234. DOI: https://doi.org/10.4038/cjs.v47i3.7530
Dan-Nwafor CC, Ogbonna U, Onyiah P, et al. Cholera outbreak in a rural north central Nigerian community: an unmatched case-control study. BMC Public Health. 2019;19:112. DOI: https://doi.org/10.1186/s12889-018-6299-3
D’Mello-Guyett L, Greenland K, Bonneville S, et al. Distribution of hygiene kits during a cholera outbreak in Kasaï-Oriental, Democratic Republic of Congo: a process evaluation. Conflict and Health. 2020;14:51. DOI: https://doi.org/10.1186/s13031-020-00294-w
Gabutti G, Rossanese A, Tomasi A, et al. Cholera, the current status of cholera vaccines and recommendations for travelers. Vaccines. 2020;8:1-17. DOI: https://doi.org/10.3390/vaccines8040606
Gidado S, Awosanya E, Haladu S, et al. Cholera outbreak in a naïve rural community in Northern Nigeria: the importance of hand washing with soap, September 2010. PAMJ. 2018;30:5. DOI: https://doi.org/10.11604/pamj.2018.30.5.12768
Humphries RM, Linscott AJ. Laboratory diagnosis of bacterial gastroenteritis. Clin Microbiol Rev. 2015;28:3-31. DOI: https://doi.org/10.1128/CMR.00073-14
Jiang L, Ng IHL, Hou Y, et al. Infectious disease transmission: survey of contacts between hospital-based healthcare workers and working adults from the general population. J Hosp Infect. 2018;98:404e411. DOI: https://doi.org/10.1016/j.jhin.2017.10.020
Llanes L, Somarriba L, Velázquez B, et al. Low prevalence of Vibrio cholerae O1 versus moderate prevalence of intestinal parasites in food handlers working with health care personnel in Haiti. Pathog Glob Health. 2016;110:30-32. DOI: https://doi.org/10.1080/20477724.2016.1141471
Malangu N, Legothoane A. Analysis of occupational infections among health care workers in Limpopo Province of South Africa. Glob J Health Sci. 2012; 5:44-51. DOI: https://doi.org/10.5539/gjhs.v5n1p44
Marin MA, Thompson CC, Freitas FS, et al. Cholera outbreaks in Nigeria are associated with multidrug resistant atypical El Tor and Non-O1/Non-O139 Vibrio cholerae. PLoS Negl Trop Dis. 2013;7:e2049. DOI: https://doi.org/10.1371/journal.pntd.0002049
Nsagha DS, Atashili J, Fon PN, et al. Assessing the risk factors of cholera epidemic in the Buea Health District of Cameroon. BMC Public Health. 2015;15:1-7. DOI: https://doi.org/10.1186/s12889-015-2485-8
Oladele DA, Oyedeji KS, Niemogha MT, et al. An assessment of the emergency response among health workers involved in the 2010 cholera outbreak in northern Nigeria. J Infect Public Health. 2012;5:346-353. DOI: https://doi.org/10.1016/j.jiph.2012.06.004
Park JM, You Y-H, Cho H-M, et al. Food borne infectious diseases mediated by inappropriate infection control in food service businesses and relevant counter measures in Korea. Osong Public Health Res Perspect. 2017; 8:159-168. DOI: https://doi.org/10.24171/j.phrp.2017.8.3.02
Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6:14-17.
Rabbani GH, Greenough WB. Food as a vehicle of transmission of cholera. Journal of Diarrheal Dis Res. 1999;17:1-9.
Swaddiwudhipong W, Hannarong S, Peanumlom P, et al. Two consecutive outbreaks of food-borne cholera associated with consumption of chicken rice in northwestern Thailand. Southeast Asian J Trop Med Public Health. 2012;43:927-932.
Tamason CC, Tulsian SM, Siddique AK, et al. What is cholera? A preliminary study on caretakers’ knowledge in Bangladesh. J Health, Popul Nutr. 2016;35:3. DOI: https://doi.org/10.1186/s41043-016-0040-6
Tian L, Zhu X, Chen Z, et al. Characteristics of bacterial pathogens associated with acute diarrhea in children under 5 years of age: a hospital-based cross-sectional study. BMC Infect Dis. 2016;16:253. DOI: https://doi.org/10.1186/s12879-016-1603-2
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/mm.2021.10058
https://doi.org/10.4081/mm.2021.10058



