Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Autologous peripheral blood mononuclear cells for the treatment of lower extremity lymphedema: a preliminary report
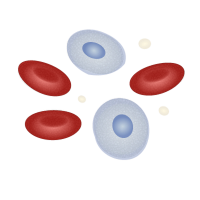
Lymphedema is a chronic devastating disease characterized by the accumulation of fluid in the extremities, tissue progressive changes such as adipose tissue deposition and fibrosis. To restore the functionality and structural integrity of the damaged lymphatic vessels, autologous peripheral blood mononuclear cells (PBMNC) was implanted in 3 sessions, 4 weeks apart, in the affected limb. Each patient was followed for 6 months, monitoring changes in the limb volume. Lymphangiogenesis was evaluated by lymphoscintigraphy, and the monitoring of quality of life. A rapid reduction in the volume of the limbs was observed: 24.5% of volume reduction after the first implant, 18.5% after the second, and 15.3% at 6 months after the third (p<0.05 vs baseline).
Lymphoscintigraphy showed a hyper fixation of the tracer along the ipsilateral iliac axis not appreciable at baseline. Implants of autologous PBMNC in patients with primary lower limb lymphedema seems to be a feasible, effective therapy option.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/vl.2021.10016
https://doi.org/10.4081/vl.2021.10016